You breathe, you absorb, you react; this is the simplified cycle of how your body deals with the environment around you, including the smoke from cigarettes. As a smoker, or even as someone regularly exposed to second-hand smoke, you’ve likely heard about the various health risks associated with the habit. However, the intricate ways in which smoking reshapes your immune system’s response to threats might be less familiar territory. From altering the delicate balance of immune cells to the disruption of critical signaling pathways, smoking weaves its influence deep within your body’s defenses. As we look closer, you’ll find that the impact extends beyond the commonly discussed respiratory issues, potentially redefining your understanding of the body’s ability to protect itself against diseases. What emerges is a nuanced picture of vulnerability, one where the embers of a cigarette have far-reaching consequences that could compromise your health in unexpected ways.
Key Takeaways
- Smoking disrupts immune function and alters the development and function of T cells.
- Smoking compromises the body’s ability to combat infections, particularly in the respiratory tract.
- The alterations in immune response caused by smoking can lead to autoimmune reactions.
- Chronic inflammation caused by smoking can result in tissue damage and contribute to various diseases.
Smoking and Immune System Basics

Understanding how smoking disrupts the immune system begins with recognizing its adverse effects on the cellular mechanisms governing immune responses. As you’re keenly aware, tobacco smoking is not only a global health menace but also a potent disruptor of immune function. Smokers are subjected to a barrage of harmful substances that can provoke inflammatory responses and impair the immune system’s ability to combat infections, particularly in the respiratory tract.
The constituents of cigarette smoke, including carcinogens like nicotine, formaldehyde, and ammonia, act as double-edged swords—they serve as pro-inflammatory agents while also wielding immunosuppressive effects. This duality is detrimental to maintaining a balanced immune response. Smoking alters the development and function of T cells, critical components of the adaptive immune response. It affects cytokine production and disrupts the effector functions of both T helper cells and CD8+ T cells, which are essential for responding to pathogens and malignancies.
Moreover, smoking’s impact reaches the innate immune system as well. It alters the number, distribution, and function of dendritic cells and Langerhans cells, which are pivotal in antigen presentation and the initiation of the immune response. The upregulation of IL-33 from epithelial cells due to tobacco exposure is a testament to its capacity to trigger acute inflammation through toll-like receptors.
The complexity of smoking’s influence extends to its variable effects on Th17 cells, which can exacerbate conditions like Crohn’s disease. Collectively, these effects of cigarette smoking contribute to the development of chronic diseases such as chronic obstructive pulmonary disease (COPD), a testament to smoking’s capacity to inflict long-term damage on the immune system.
Adaptive Immunity Alterations
Cigarette smoking significantly impairs adaptive immunity by altering the development and function of key cells such as T and B lymphocytes, which are crucial for a targeted immune response. These alterations can have profound effects on your ability to fight infections and respond to vaccines, as well as implications for the development of immune-related diseases.
To paint a detailed picture of the impact smoking has on adaptive immunity, consider the following:
- Cytotoxic T Lymphocyte Impairment: CD8+ T cells, or cytotoxic T lymphocytes, are essential for killing virus-infected cells and tumor cells. Smoking disrupts the maturation and effector function of these cells, compromising your body’s ability to effectively eliminate such threats.
- T Helper Cell Dysfunction: T helper cells orchestrate the immune response. Smoking skews the balance between different subsets of T helper cells, like increasing Th17 in COPD patients, which can disrupt immune homeostasis and exacerbate certain conditions.
- Regulatory T Cell Alteration: The immunosuppressive function of Tregs (regulatory T cells) is intended to prevent autoimmune reactions. However, smoking modifies their function, potentially leading to an inadequate or overreactive immune response.
- Altered Cytokine Production: Cigarette smoke exposure results in altered cytokine profiles, which can misguide the immune response. The disruption in cytokine signaling can lead to a reduced response to pathogens and impaired communication between the innate and adaptive immune systems.
These adaptive immunity alterations can hinder your ability to serve others in healthcare settings by increasing susceptibility to infections and reducing the effectiveness of immunizations. Understanding these changes can inform strategies to mitigate the impact of smoking on the immune system and improve patient outcomes.
Innate Immune Function Disruption
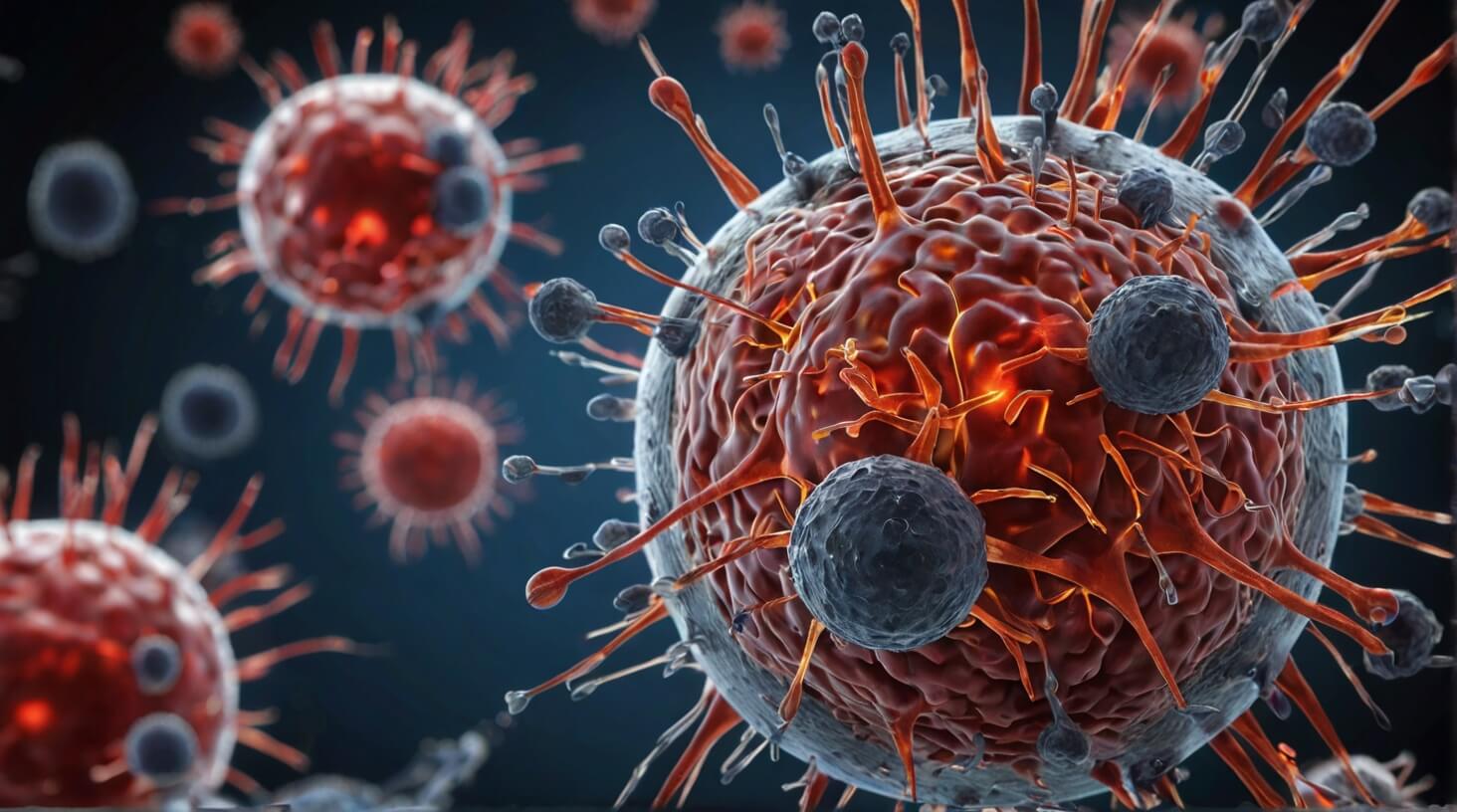
While smoking’s detrimental effects on adaptive immunity are clear, it’s equally important to recognize how it disrupts innate immune function, the body’s first line of defense against pathogens. Cigarette smoke exposure (CSE) is notorious for its cigarette smoke-induced alterations in the innate immune system. Specifically, CSE instigates acute inflammation through the activation of toll-like receptors, which hampers the functionality of dendritic cells and Langerhans cells, both pivotal to the innate immune responses.
Moreover, cigarette smoke enhances the release of IL-33 from epithelial cells and concurrently alters the expression of the IL-33 receptor ST2 on immune cells. This dysregulation can skew innate immune responses, leading to an increased susceptibility to infections and impaired wound healing. Chronic tobacco smoke is a well-known risk factor for chronic obstructive pulmonary disease (COPD) and other lung diseases, where it not only causes mucosal inflammation but also impacts immune homeostasis through oxidative stress and the heightened expression of inflammatory cytokines.
Alveolar macrophages, the lung’s resident phagocytes, exhibit compromised phagocytic activity in the presence of cigarette smoke, which is essential for the eradication of pathogens and debris. Furthermore, cigarette smoke suppresses the function of natural killer (NK) cells, a crucial component of the host defense against tumor cells and virally infected cells.
Molecular Pathways and Smoking

Delving into the molecular pathways affected by smoking reveals that tobacco smoke components, such as nicotine, significantly disrupt T cell development and cytokine production, compromising the body’s immune response. You’ll uncover that cigarette smoke extract interacts with immune cells through various mechanisms, leading to a cascade of detrimental effects. Here are some pivotal points:
- Cigarette Smoke and T Cells: Smoking skews the differentiation of T cells, increasing the percentage of Th17 cells, particularly in individuals with COPD. This shift toward Th17 cells is associated with increased expression of pro-inflammatory cytokines, which exacerbates the inflammatory response.
- Nicotinic Acetylcholine Receptors: Nicotine from cigarette smoke binds to nicotinic acetylcholine receptors (nAChRs), including the α7 nicotinic acetylcholine subtype, altering signaling pathways within immune cells. The interaction with α7 nAChRs can lead to immunosuppressive effects, hindering the body’s ability to combat infections and increasing susceptibility to diseases.
- Oxidative Stress: Reactive oxygen species (ROS) generated by cigarette smoke contribute to oxidative stress, which can damage proteins, lipids, and DNA in immune cells. This stress can activate the receptor for advanced glycation end products, further impairing immune function.
- Th2 Immune Responses: Exposure to tobacco smoke also affects Th2 immune responses, which are crucial for fighting parasitic infections and are implicated in allergic reactions. Smoking has been linked to the dysregulation of Th2 responses, which may underlie the increased incidence of asthma and allergies among smokers and those exposed to secondhand smoke.
As someone committed to serving others, understanding these molecular interactions is vital for addressing the impact of smoking on immune function and for supporting individuals with smoking-related conditions such as COPD.
Smoking-Related Immunopathologies
Understanding the molecular disruptions caused by smoking, let’s examine how these alterations contribute to smoking-related immunopathologies, including chronic inflammation and autoimmune responses. Your role, dedicated to aiding others, requires a grasp of the complex interplay between tobacco smoke exposure and the immune system.
Cigarette smoke impacts both innate and adaptive immunity, skewing the balance and function of immune cells. Macrophages and neutrophils, crucial to innate defenses, are overactivated by smoking, leading to an enhanced chronic inflammatory state. This dysregulation results in a heightened cytokine response, with an increase in pro-inflammatory mediators that perpetuate tissue damage and sustain chronic inflammation.
Adaptive immunity, characterized by T cell development and cytokine production, is also altered. Smoking increases the prevalence of Th17 and Th1 cells, which are intimately involved in the pulmonary inflammation witnessed in smokers. The effects of cigarette smoke on these cells contribute to the risk of respiratory infections and chronic autoimmune conditions like Crohn’s disease and colitis.
Furthermore, tobacco smoke exposure affects other adaptive immune cells, exacerbating Th2-mediated airway inflammation. The immune and inflammatory mediators produced in response to smoking can worsen conditions such as asthma and chronic obstructive pulmonary disease (COPD).
At the molecular level, cigarette smoke enhances IL-33 release, modulates toll-like receptor responses, and impacts dendritic cell subsets, pivotal in dictating the course of innate immunity. These effects of chronic smoking create an environment conducive to the development and exacerbation of immunopathologies.
As you continue to serve those affected, understanding the link between smoking and immune dysregulation is vital for informing prevention strategies and targeted therapies.