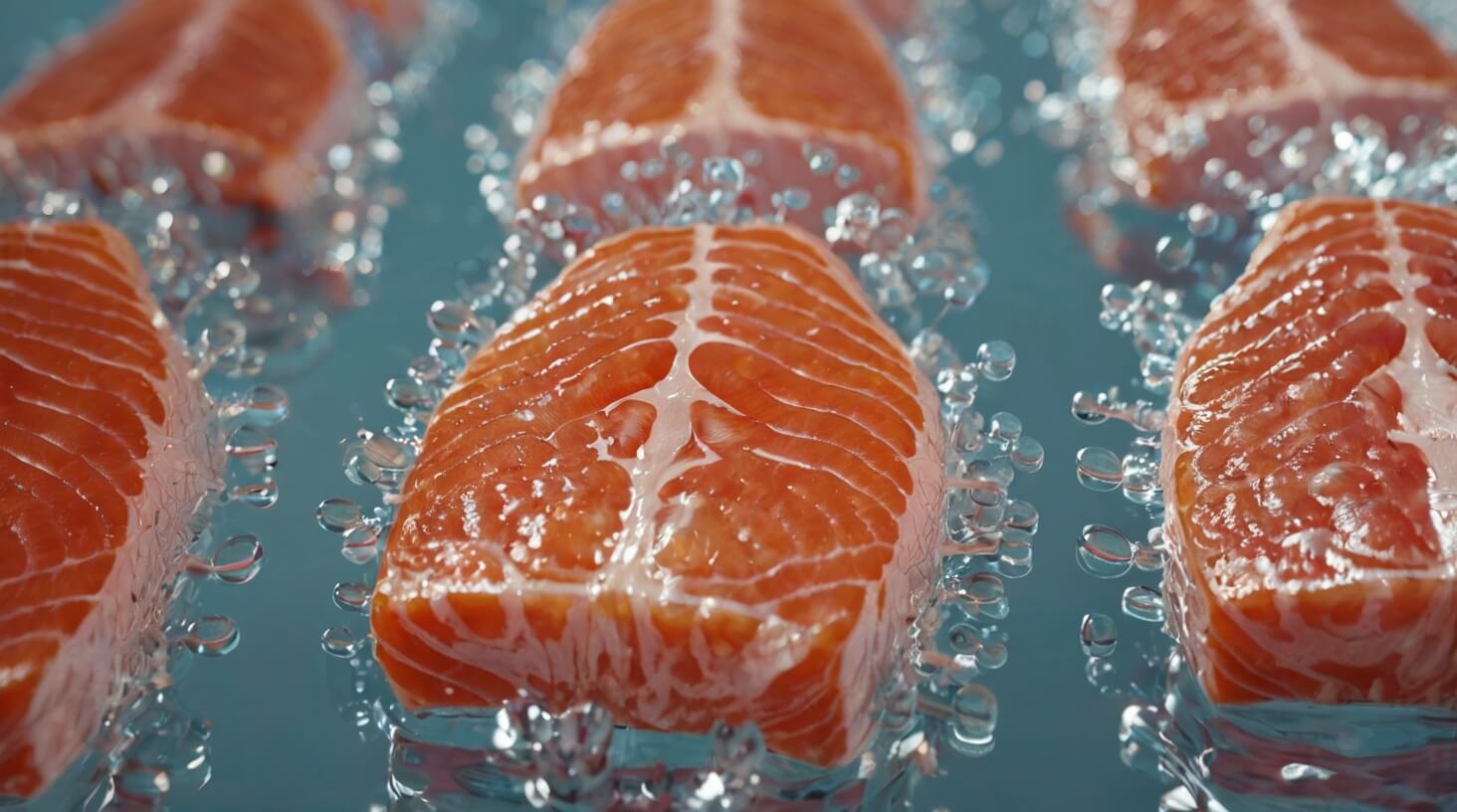
Just as you’re pondering the intricacies of your body’s defense mechanisms, it turns out that the immune response, a complex system crucial for your health, might be significantly influenced by something as simple as the fats in your diet. You’ve likely heard about Omega-3 fatty acids, but you may not fully appreciate their potential role in modulating inflammation and supporting immune function. These essential fats, abundantly found in fish oils, flaxseeds, and walnuts, are not just beneficial for your heart; they’re also vital players in the intricate game of immune regulation. By incorporating Omega-3s into your diet, you’re potentially steering your immune cells towards a more regulated and less overzealous reaction to threats. However, the depth of their influence and the mechanisms behind their effects on specific immune cells like macrophages, T cells, and B cells are a fascinating puzzle that’s still being pieced together. So, consider the implications of Omega-3s on your well-being and how they might just be a key factor in maintaining your body’s equilibrium in the face of environmental assaults.
Key Takeaways
- Omega-3 fatty acids alter immune cell membrane composition and modulate cytokine production.
- Omega-3s favor the production of anti-inflammatory cytokines and inhibit migration of neutrophils to inflamed tissues.
- Omega-3s impact macrophage activity, influencing cytokine and chemokine production, membrane fluidity, and polarization.
- Omega-3s enhance the phagocytic capacity of neutrophils and have a broader role in the immune landscape, affecting T cells and B cells.
Omega-3s and Inflammation Reduction

Omega-3 fatty acids play a pivotal role in dampening the body’s inflammatory response through mechanisms that include altering immune cell membrane composition and modulating cytokine production. These essential fatty acids, primarily eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are integral to maintaining homeostasis within the immune system. By integrating into the cellular membranes of immune cells, omega-3 fatty acids facilitate a fluid and responsive environment conducive to mitigating excessive inflammatory reactions.
You’ll find that fish oil supplementation, a rich source of EPA and DHA, has been associated with the production of specialized pro-resolving mediators (SPMs). These SPMs, including resolvins and protectins, are pivotal in orchestrating the termination phase of inflammation. They not only reduce inflammation but also promote the clearance of inflammatory debris, thus supporting tissue healing and resolution.
The anti-inflammatory effects of omega-3 fatty acids extend to the modulation of macrophage function. Macrophages treated with omega-3 fatty acids exhibit altered cytokine profiles, favoring the production of anti-inflammatory rather than pro-inflammatory cytokines. Moreover, these fatty acids enhance phagocytosis, the process by which macrophages engulf and digest cellular debris and pathogens, which is essential for the resolution of inflammation.
Furthermore, omega-3 fatty acids influence neutrophil function. They inhibit migration of neutrophils to inflamed tissues, which is a critical step in the inflammatory process. In addition, omega-3 fatty acids can temper the production of reactive oxygen species from neutrophils, reducing potential tissue damage.
In essence, omega-3 fatty acids and their metabolites serve as modulators within the immune system, acting to restore balance and prevent the escalation of inflammatory responses. Their role in immune regulation suggests significant therapeutic potential in conditions characterized by chronic inflammation.
Modulating Macrophage Activity
While you consider the impact of diet on your health, it’s crucial to understand how the omega-3 fatty acids found in fish oil can precisely tune macrophage activity, a cornerstone of your immune system’s response. These polyunsaturated fatty acids, particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), play a pivotal role in modulating macrophage function. They are known to impact the production of cytokines and chemokines, signaling molecules that are vital in orchestrating the immune response.
EPA and DHA from omega-3 fatty acids become incorporated into the cell membrane of macrophages, fundamentally influencing their membrane fluidity and signaling pathways. This incorporation alters the landscape of the cell membrane, thus affecting the macrophage’s ability to engage in phagocytosis—the process of engulfing and digesting pathogens and cellular debris. Additionally, omega-3 fatty acids influence macrophage polarization, a process that determines the macrophage’s role as either pro-inflammatory (M1) or anti-inflammatory (M2). This is particularly relevant in the context of anti-inflammatory diseases, where an overactive immune response can be detrimental.
Furthermore, the effect of omega-3 fatty acids extends to other immune cells, such as T cells and B cells, indicating a broader role in the immune landscape. Fish oil supplementation, rich in EPA and DHA, has been shown to enhance the phagocytic capacity of neutrophils—another type of immune cell—thereby boosting an essential aspect of the immune response.
As you serve others, it’s valuable to recognize the potential of omega-3 fatty acids in supporting and modulating immune function. A diet rich in these nutrients may be a key factor in maintaining not only general health but also in managing immune-related conditions effectively.
Neutrophil Function and Omega-3s
Diving into the intricacies of neutrophil function, it’s evident that the incorporation of omega-3 fatty acids into their cell membranes significantly enhances their phagocytic abilities and cytokine production. Neutrophils, a type of white blood cells, are a crucial component of the innate immune system, and their optimal functioning is vital for your body’s first line of defense against infection. Omega-3 fatty acids, particularly EPA and DHA, play a significant role in modulating this aspect of immune function.
To capture the significance of omega-3s in neutrophil activity, consider the following points:
- Phagocytic Capacity Increase: Omega-3 fatty acids, especially DHA, boost the ability of neutrophils to engulf and destroy pathogens.
- Regulation of Inflammation: The anti-inflammatory effects of omega-3-derived metabolites help in resolving inflammation more effectively.
- Enhanced Neutrophil Adhesion: Proper neutrophil adhesion is essential for targeted immune responses, and EPA and DHA can influence this process.
- Production of Resolving Mediators: Through competition with omega-6 fatty acids, omega-3s lead to the synthesis of specialized pro-resolving mediators that regulate immune responses.
The dynamics of inflammation and immune function can be positively influenced by dietary supplementation with fish oil, rich in EPA and DHA. Such supplementation has been shown to increase the phagocytic capacity of neutrophils in human blood. This is significant because it not only enhances your innate immune system’s ability to fight infections but also modulates the inflammatory response, potentially reducing chronic inflammation in various diseases.
T Cell Response to Omega-3s
Building on the understanding of how neutrophils benefit from omega-3 fatty acids, it’s crucial to explore how these nutrients similarly enhance T cell function within the adaptive immune system. The incorporation of omega-3 fatty acids, particularly EPA and DHA, into T cell membranes is a pivotal factor. It affects their fluidity and, consequently, their signaling capabilities, which are fundamental for T cell activation and function.
Research indicates that omega-3 fatty acids can regulate the differentiation and proliferation of T cells. This is particularly evident in CD8+ T cells, which are essential for targeting and eliminating infected cells. High EPA blood levels correlate with a modulated immune response, often marking a shift toward less inflammatory states.
The effects of DHA on T cell response are also noteworthy. DHA can influence the balance between different types of T cells, such as helper T cells and regulatory T cells, thus impacting overall immune responses. To illustrate this, consider the following table, which summarizes key interactions between omega-3 fatty acids and T cells:
| Omega-3 Fatty Acid | T Cell Aspect Affected | Immune Response Outcome |
|---|---|---|
| EPA | CD8+ T cell activation | Modulated immune responses |
| DHA | T cell differentiation | Balanced regulatory effects |
| General Omega-3s | Membrane incorporation | Enhanced cellular signaling |
As you aim to serve others through health education or clinical practice, understanding these interactions is essential. Omega-3s are not just nutrients; they’re active participants in the immune symphony, fine-tuning the responses of immune cells for optimal performance. Encouraging optimal EPA and DHA intake could be a strategic part of managing immune health, potentially shaping more effective, controlled immune responses.
B Cell Activation Dynamics
Understanding the dynamics of B cell activation is critical, as it encompasses the process by which B cells recognize antigens, proliferate, and differentiate into antibody-producing plasma cells. This complex sequence ensures your immune system remains vigilantly poised to defend against pathogens and, when necessary, promote tissue repair.
In the context of how omega-3 fatty acids influence B cell activation, the following points are particularly noteworthy:
- Omega-3 fatty acids, particularly DHA and EPA, can alter membrane composition, potentially affecting B cell receptor organization and signaling.
- These fatty acids may modulate the production of cytokines, which are vital for B cell activation and differentiation.
- Higher plasma levels of omega-3s have been associated with an enhanced production of antibodies after vaccination, suggesting a role in promoting optimal immune responses.
- The anti-inflammatory properties of omega-3 fatty acids could help maintain immune balance, preventing overactivation of B cells that can lead to autoimmune conditions.
Omega-3 fatty acids, found in fish oil and certain plant oils, are not just nutritional supplements; they’re integral to modulating your immune responses. Studies reveal that these fats can impact B cells at several junctures. By influencing membrane composition, omega-3 fatty acids may affect how B cells detect antigens. It’s a bit like fine-tuning a radio; the right membrane composition ensures B cells are tuned to the correct frequency to detect invaders.
Moreover, the interplay between fatty acids and the immune system is not a one-way street. Adequate vitamin D levels, often found alongside omega-3s, are pivotal for maintaining the immune system, including B cell function.
In serving others, it’s essential to appreciate how dietary components like omega-3 fatty acids can be leveraged to support an optimal immune system, including the nuanced activation dynamics of B cells.
Omega-3 Impact on Immune Cells

Omega-3 fatty acids frequently modulate the functionality of various immune cells, playing a pivotal role in both innate and adaptive immune responses. These essential nutrients, often derived from fish oils, have a remarkable capacity to alter cell function, particularly by competing with omega-6 fatty acids for enzymes crucial in the synthesis of bioactive metabolites. This competition is a delicate balance that significantly affects the activity and efficiency of immune cells.
When it comes to macrophages, omega-3 fatty acids influence their function by modulating cytokine and chemokine production. This alteration can lead to changes in macrophage polarization, swinging the balance towards an anti-inflammatory state beneficial for chronic inflammatory conditions. The incorporation of omega-3 fatty acids, namely eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), into the lipid rafts of immune cell membranes is particularly critical. This integration affects the fluidity and molecular composition of the membranes, which in turn influences immune cell activation, proliferation, and antibody production.
Neutrophils, another key player in the immune system, also experience the impact of omega-3 fatty acids. Their function, including migration, phagocytic capacity, and cytokine production, is affected by the presence of these fatty acids. The metabolites of EPA and DHA can act as anti-inflammatory agents, further contributing to a regulated immune response.
In essence, omega-3 fatty acids provide a regulatory effect on the immune system. By modifying immune cell behavior and the production of cytokines, they contribute to a balanced immune response. These effects underscore the importance of omega-3 fatty acids in maintaining immune health and their potential therapeutic applications in immune-related disorders.