Inflammation is the match that lights the fire within your body, sometimes burning uncontrollably and spreading its effects far beyond the initial spark. When you encounter peripheral infections or suffer trauma, your body’s inflammatory response doesn’t always stay localized; it can have profound and often underappreciated consequences on your brain function. You’ve likely heard about the impact of inflammation on physical health, but have you considered its subtle and not-so-subtle influence on your cognitive abilities, mood, and neurological health? As scientists uncover the intricate pathways through which inflammation can disrupt the sanctity of the blood-brain barrier and interfere with neural processes, you must wonder how this silent intruder affects the very essence of your being. The next time you feel a bit foggy after fighting off an infection, you might start to question whether the battlefields of your body’s defense systems have extended into the territory of your mind, suggesting a hidden war that warrants a closer look.
Key Takeaways
- Neuroinflammation is a critical mechanism for neural protection and repair.
- Chronic inflammation in neurodegenerative diseases like Alzheimer’s and Parkinson’s can damage neurons and disrupt synaptic function.
- Genetic factors such as CD33 and TREM2 variants influence microglial response to Alzheimer’s pathology.
- Inflammatory responses mediated by microglia and astrocytes are linked with cognitive decline.
Understanding Neuroinflammation
To grasp neuroinflammation’s impact on brain function, it’s essential to understand how microglia and astrocytes orchestrate this complex immune response within the central nervous system. Microglial cells, as the primary brain’s immune cells, serve as the first line of defense, constantly surveilling the neural environment. When they detect a threat, they transform, adopting an amoeboid shape that allows them to phagocytose pathogens and cellular debris. Astrocytes, while traditionally viewed as support cells, contribute significantly to neuroinflammation by releasing proinflammatory cytokines that modulate microglial activity.
You should note that neuroinflammation is not inherently deleterious; it is a critical mechanism for neural protection and repair. However, the chronic inflammation that is characteristic in neurodegenerative diseases like Alzheimer’s and Parkinson’s can be detrimental. The inflammatory response, when unregulated, leads to the excessive release of proinflammatory cytokines and other toxic substances that can damage neurons and disrupt synaptic function.
Moreover, genetic factors such as CD33 and TREM2 variants influence how microglial cells respond to amyloid plaques and tau tangles, key features of Alzheimer’s pathology. These genetic variations can either mitigate or exacerbate the inflammatory response, thus affecting disease progression.
The integrity of the blood-brain barrier is also vital in the context of neuroinflammation. In a healthy state, this barrier protects the brain from systemic infections. However, during neuroinflammation, its permeability can increase, allowing immune cells and inflammatory mediators from the peripheral system to infiltrate the central nervous system, potentially worsening brain inflammation.
Understanding the evolutionary basis of neuroinflammation is paramount in designing targeted therapies that modulate microglial and astrocytic function to treat or prevent neurodegenerative diseases. Your objective is to advance this understanding to serve those afflicted by such conditions, by developing strategies that harness the protective aspects of neuroinflammation while mitigating its harmful effects.
Cognitive Impairment Links
Building on the understanding of neuroinflammation, it’s crucial to explore how this process contributes to cognitive impairment and the development of neurodegenerative diseases. The inflammatory responses within the brain, particularly those mediated by brain’s immune cells such as microglia and astrocytes, are intimately linked with cognitive decline. These cells, when activated inappropriately or excessively, can release a cascade of inflammatory mediators that adversely affect cognitive function.
The nexus between chronic inflammation in the brain and cognitive impairment is not merely correlative but indicates a more direct pathological role. Genetic predispositions, for instance, mutations in genes like CD33 and TREM2, significantly modulate neuroinflammatory responses. Such genetic factors can predispose individuals to an increased risk of dementia by altering the way inflammation is handled in the brain.
Systemic inflammation, which may arise from chronic stress, infections, or diseases, also plays a detrimental role. It can breach the protective blood-brain barrier, leading to a milieu that can exacerbate cognitive symptoms. This systemic-to-brain inflammatory signaling underscores the importance of addressing peripheral inflammation for maintaining cognitive performance.
Understanding the dynamics of neuroinflammation and its effect on cognitive decline is pivotal for health professionals who aim to serve and improve patient outcomes. It informs the development of targeted interventions to mitigate the risk factors associated with cognitive impairment. Thus, in your role dedicated to serving others, you’re empowered to advocate for and implement strategies that may reduce inflammation and preserve cognitive health, ultimately reducing the burden of neurodegenerative diseases in the community.
Mood Disorders and Inflammation

Emerging research reveals that mood disorders such as depression and anxiety are frequently accompanied by increased levels of systemic inflammation, implicating this biological response as a potential contributor to the pathophysiology of these conditions. As you delve into the interplay between the brain and inflammation, it’s crucial to understand the role of the immune system in modulating mood and cognitive functions.
Chronic inflammation can act as a catalyst for mood disorders by disrupting the delicate balance of neurotransmitters and impeding neurogenesis, which is vital for mood regulation. Inflammatory cytokines, which are part of the immune responses, can cross the blood-brain barrier and alter brain function, leading to depressive symptoms. This understanding underscores the need for interventions aimed at reducing systemic inflammation to mitigate the risk of mood disorders.
To illustrate the relationship between mood disorders and inflammation, consider the following table:
| Factor | Impact on Mood Disorders | Intervention |
|---|---|---|
| Chronic Inflammation | Exacerbates symptoms of depression and anxiety | Lifestyle modifications, NSAIDs |
| Immune System Dysregulation | Leads to imbalanced immune responses affecting brain function | Immunomodulatory drugs |
| Neurotransmitter Imbalance | Impairs mood regulation | Addressing underlying inflammation |
| Impaired Neurogenesis | Reduces resilience to stress, affecting emotional well-being | Promoting anti-inflammatory habits |
| Cognitive Dysfunction | Contributes to the severity of mood disorders | Comprehensive treatment strategies |
Addressing inflammation through a multi-faceted approach, including medical and lifestyle interventions, is paramount. Encouraging patients to adopt anti-inflammatory diets, engage in regular physical activity, manage stress effectively, and maintain optimal sleep hygiene can serve as foundational strategies. Additionally, pharmacological agents such as NSAIDs or more targeted immunomodulatory therapies may be necessary for treating underlying inflammatory processes that contribute to mood disorders. Your role in serving patients involves a precise understanding of these dynamics and the implementation of tailored treatment plans to address the complex interplay between systemic inflammation and mood dysregulation.
Neurological Diseases Connection
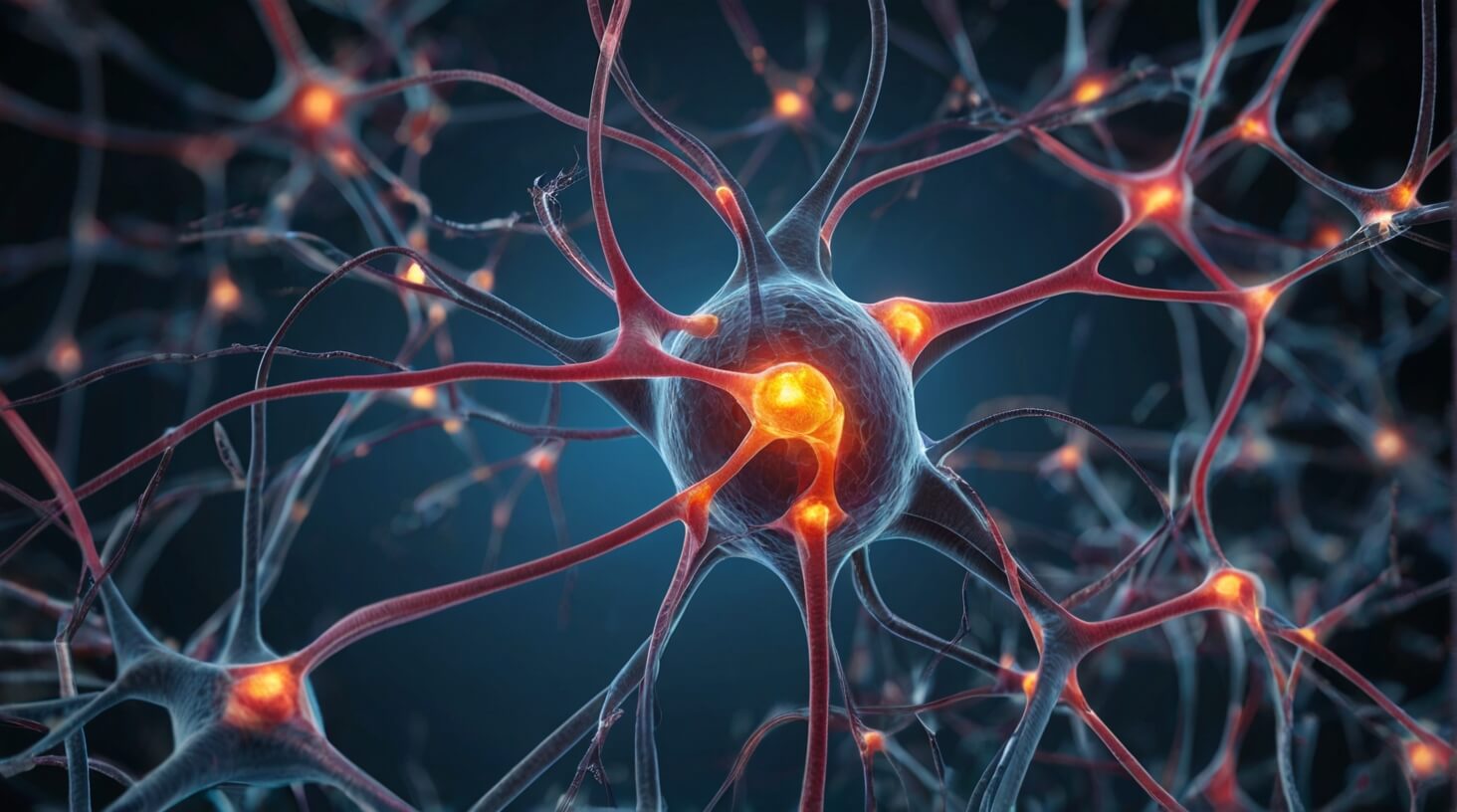
Neuroinflammation frequently plays a central role in the progression of neurological diseases such as Alzheimer’s and Parkinson’s, altering essential brain functions and exacerbating cognitive decline. Alzheimer’s disease pathology is characterized by the accumulation of amyloid plaque and neurofibrillary tangles, which are exacerbated by the brain’s inflammatory response. Similarly, Parkinson’s disease features the presence of Lewy bodies, and higher levels of inflammatory processes are implicated in its progression.
Your understanding of these conditions is crucial to providing compassionate care. The gene CD33 acts as an ‘on switch’ for Alzheimer’s-associated neuroinflammation, while the TREM2 mutation can trigger microglia to adopt an inflammatory state, a commonality in both Alzheimer’s and Parkinson’s. The chronic diseases of the mind, worsened by inflammation, demand a proactive approach to management and intervention.
Crucially, excessive neuroinflammation correlates with cognitive decline and an elevated risk for age-related cognitive impairments. Systemic inflammation can alter the blood-brain barrier, a critical defense against pathogens, potentially leading to further neuronal damage. Addressing inflammation is not just about alleviating immediate symptoms; it’s about preserving the integrity of brain function over time.
Your role is to understand these mechanisms, as chronic inflammation can catalyze memory issues and cognitive deficits. By recognizing the signs of inflammatory patterns in your patients, you can better serve their needs and potentially delay the progression of these debilitating conditions. With an aging population, the prevalence of these neurodegenerative illnesses is set to rise, making your dedication to mitigating inflammation all the more essential for the well-being of those you serve.
Managing Inflammatory Responses
Understanding the pivotal role of inflammation in neurological conditions underscores the importance of strategic lifestyle choices to manage inflammatory responses effectively. Inflammation throughout the body, including within the brain, can be modulated by adopting a diet abundant in anti-inflammatory foods such as fruits and vegetables. These dietary choices combat immune activation and the increased levels of inflammatory cytokines that resident immune cells secrete.
Regular exercise is not merely a cornerstone of physical health but also vital in managing inflammatory responses. Physical activity has been shown to exert a systemic anti-inflammatory effect, which extends to brain tissue, potentially mitigating the risk of inflammatory disease in the central nervous system.
Furthermore, engaging in stress-reduction techniques like meditation and yoga directly addresses the inflammatory processes exacerbated by stress. Stress-induced inflammation is particularly concerning within the brain, where it can impact cognitive functions and accelerate the aging process. These practices promote a balanced immune response, lessening the potential for harmful overactivation.
Avoiding smoking and limiting alcohol consumption are also critical measures. Smoking is a well-known pro-inflammatory habit, and excessive alcohol can trigger chronic inflammation. Hence, cessation and moderation are prudent steps in managing inflammatory responses.
Lastly, prioritizing sufficient sleep is paramount. Sleep is a physiological reset for the body, during which inflammatory markers decrease. Chronic sleep deprivation, conversely, has been linked to heightened inflammatory activity.