Imagine you’re recovering from a recent bout of gastroenteritis; your gut has been through the wringer, and it’s not just the discomfort that’s been troubling you, but also a nagging sense of fatigue and vulnerability to every cold going around. This isn’t coincidence. Your gut health is intricately linked to your immune system, a connection that scientists are increasingly understanding to be as crucial as it is complex. The trillions of microbes residing in your gut, collectively known as the microbiota, play an instrumental role in educating and regulating your immune cells, shaping your body’s defense mechanisms from within. As you navigate your recovery, you might not realize that the balance of these tiny inhabitants in your gut could be the key not just to overcoming your current symptoms, but also to fortifying your immune response against future invasions. But how exactly does this microscopic ecosystem within you wield such influence over your wellbeing, and what can you do to harness its power? Let’s explore the unseen world that lives within and the silent war it wages on your behalf.
Key Takeaways
- Gut microbiota plays a crucial role in educating and regulating the immune system.
- Dysbiosis, an imbalance in the gut microbiota, can disrupt immune function and contribute to autoimmune diseases.
- The gut microbiota-derived metabolites, such as short-chain fatty acids (SCFAs), have a significant impact on immune responses.
- Maintaining a balanced diet, promoting the growth of SCFA-producing bacteria, and managing stress are essential for gut health and supporting a well-balanced immune system.
Understanding Gut Microbiota

Delving into the complex ecosystem of the gut microbiota, we find a vast array of microorganisms that play a pivotal role in maintaining our immune system’s balance. Residing within the gastrointestinal tract, the gut microbiota comprises bacteria, archaea, viruses, and fungi, all of which are integral to various physiological processes, particularly the modulation of the host’s immune system. Commensal bacteria within this collection are key in educating and regulating both innate and adaptive immunity.
You’ll observe that the interaction between the gut microbiota and immune system is intricate and dynamic. Gut microbes stimulate the development and function of intestinal immune cells, which in turn, keep the microbial communities in check. This mutualistic relationship facilitates the mucosal immune system’s ability to distinguish between harmful pathogens and beneficial microorganisms. Disruptions in this equilibrium, known as dysbiosis, can lead to immune dysregulation and the onset of autoimmune disorders.
Advancements in next-generation sequencing technology have shed light on the complexity of the gut microbiota and its role in immune-related diseases. Studies utilizing germ-free models underscore the significance of gut microbiota in shaping immune responses. Without exposure to these microorganisms, both innate and adaptive immune systems exhibit underdevelopment and functional deficits.
The implications are clear: a balanced gut microbiota is crucial for a well-functioning immune system. As you aim to serve others in the health sector, understanding the symbiotic relationship between these gut microbes and the host’s immune defenses is essential. This knowledge equips you to address dysbiosis and its potential link to autoimmune diseases, ultimately contributing to improved patient outcomes.
Immune System Fundamentals
To fully grasp the influence of gut health on overall well-being, it’s essential to understand the fundamentals of the immune system, which serves as the body’s robust defense mechanism against pathogens. The immune system can be broadly categorized into two arms: the innate immune system and the adaptive immune system. The innate system acts as the first line of defense, providing an immediate but non-specific response to invaders. In contrast, the adaptive immune system mounts a targeted and long-lasting defense, characterized by the development of immune memory.
The interplay between these two systems is complex and involves a variety of cells and signaling molecules. In the context of gut health:
- NK cells (Natural Killer cells) are key players in the innate immune response, capable of destroying infected or tumor cells without prior sensitization.
- Regulatory T cells are critical for maintaining immune homeostasis and preventing autoimmune responses by modulating the activity of other immune cells.
- T cell differentiation is influenced by signals from the gut microbiota, directing the development of a protective immune response or tolerance to harmless antigens.
Advancements in sequencing technology have shed light on how gut microbiota alterations can disrupt immune function and contribute to autoimmune diseases. Dysbiosis, a significant imbalance in the gut microbiota, hinders immune homeostasis and has been linked to various autoimmune conditions. Recognizing the role of gut microbiota in shaping immune responses opens avenues for novel therapeutic strategies aimed at restoring balance and promoting a healthy immune function, crucial for those committed to fostering well-being in others.
Gut-Immune System Interactions
Building on the immune system fundamentals outlined earlier, let’s now explore how the gut microbiota is instrumental in orchestrating both innate and adaptive immune responses. The intestinal microbiota, a complex ecosystem of microorganisms residing in the gut, is a central player in maintaining immune homeostasis. A healthy gut microbiome facilitates the development of immune system cells and the production of substances like secretory IgA, which protect intestinal epithelial cells from pathogens.
The microbial community in your gut directly influences the differentiation of T helper cells and fosters the generation of regulatory T cells, which are crucial for preventing autoimmune conditions. When there’s an imbalance—known as dysbiosis—in this intricate system, it can precipitate immune dysregulation, leading to inflammatory diseases and potentially sparking autoimmune disorders.
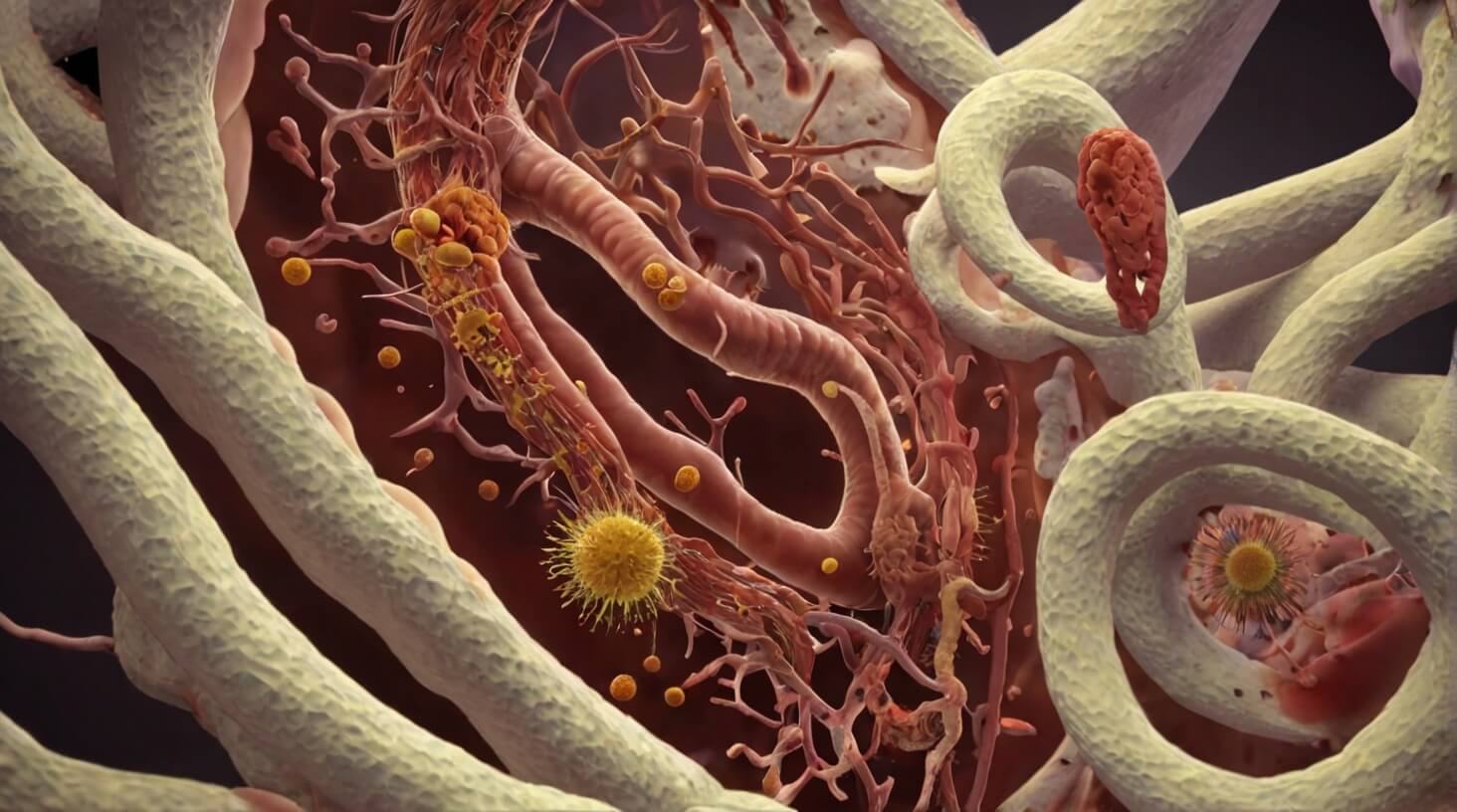
You’re keenly aware that gut microbiota-derived metabolites, such as short-chain fatty acids (SCFAs), have a profound impact on health. SCFAs, produced through the fermentation of dietary fibers by the gut flora, can modulate systemic immune responses. They play a pivotal role in maintaining the balance between pro-inflammatory and anti-inflammatory responses, which is essential for preventing chronic inflammation.
Understanding the interplay between the gut microbiome and the immune system opens doors to innovative treatments. By restoring a healthy microbial balance, it’s possible to alleviate symptoms of inflammatory diseases and, crucially, to address the root causes of immune system-related disorders. For those dedicated to serving others, recognizing the significance of gut-immune system interactions is a cornerstone of promoting holistic well-being and developing targeted interventions for autoimmune diseases.
Factors Impacting Gut Health
Numerous factors, including genetics, age, diet, and stress levels, actively shape the composition and function of your gut microbiota, with significant repercussions for your immune system’s equilibrium. Understanding these factors is essential for anyone dedicated to fostering well-being in others.
- Genetics play a foundational role, determining the initial assortment of gut bacteria that can thrive within your intestines. While you can’t change your genetic makeup, recognizing its impact on your microbiota composition is crucial for personalized approaches to health.
- Diet is a modifiable element that has profound effects on your gut microbiota. The diversity and quality of your food intake can either support a robust commensal microbiota or contribute to dysbiosis, a state linked with inflammatory bowel disease and other immune-related disorders.
- Environmental factors, including the use of antibiotics, exposure to pollutants, and lifestyle choices such as smoking and physical activity levels, are also pivotal in shaping your gut ecosystem.
Your diet, specifically, can either nourish your gut bacteria or disrupt intestinal homeostasis. High-fiber foods, prebiotics, and fermented products support a healthy microbiota, while a diet high in processed foods and sugar can lead to an imbalance, increasing disease risk. Stress, often overlooked, can trigger changes in gut bacteria, leading to a heightened inflammatory response and potentially exacerbating conditions like inflammatory bowel disease.
To maintain a well-balanced immune system, it’s imperative to consider these factors when advising on lifestyle changes or interventions. A tailored approach, taking into account individual variability in microbiota and immune system interactions, can help mitigate disease risk and promote long-term gut health.
Enhancing Immune Response

Understanding the intricate relationship between gut microbiota and the body’s immune mechanisms is pivotal for enhancing immune responses and reducing the incidence of autoimmune disorders. Your role in supporting others includes recognizing how the intestinal immune system interacts with the host immune system. The gut microbiota plays a crucial role in shaping both the innate and adaptive immune responses. By fostering beneficial bacteria through dietary choices, including probiotics and prebiotics, you can aid in the development of the immune system, promoting immune tolerance and averting dysbiosis that often precedes autoimmune diseases.
In the realm of gut health, bacterial products like short-chain fatty acids (SCFAs) are instrumental. They are byproducts of fermentation that influence the gut’s local environment and the systemic immune response. SCFAs help in maintaining the integrity of the gut barrier and modulate the function of innate immune effectors, including dendritic cells and macrophages. This interaction between microbiota and host cells encourages a balanced immune response, protecting against pathogenic invasions while preventing overreaction that could lead to autoimmunity.
To harness this knowledge for the benefit of those you serve, consider nutritional interventions that support the growth of SCFA-producing bacteria. Encourage the consumption of fiber-rich foods that act as prebiotics, fueling the beneficial microbiota. Educating individuals on the importance of a diverse microbiome can substantially influence the health outcomes associated with their immune systems.
Manipulation of gut microbiota through targeted dietary strategies not only holds promise for the treatment of autoimmune diseases but also represents a proactive approach to enhancing overall immune function. This proactive strategy equips individuals with the power to influence their health, potentially offsetting the development of immune-related conditions.