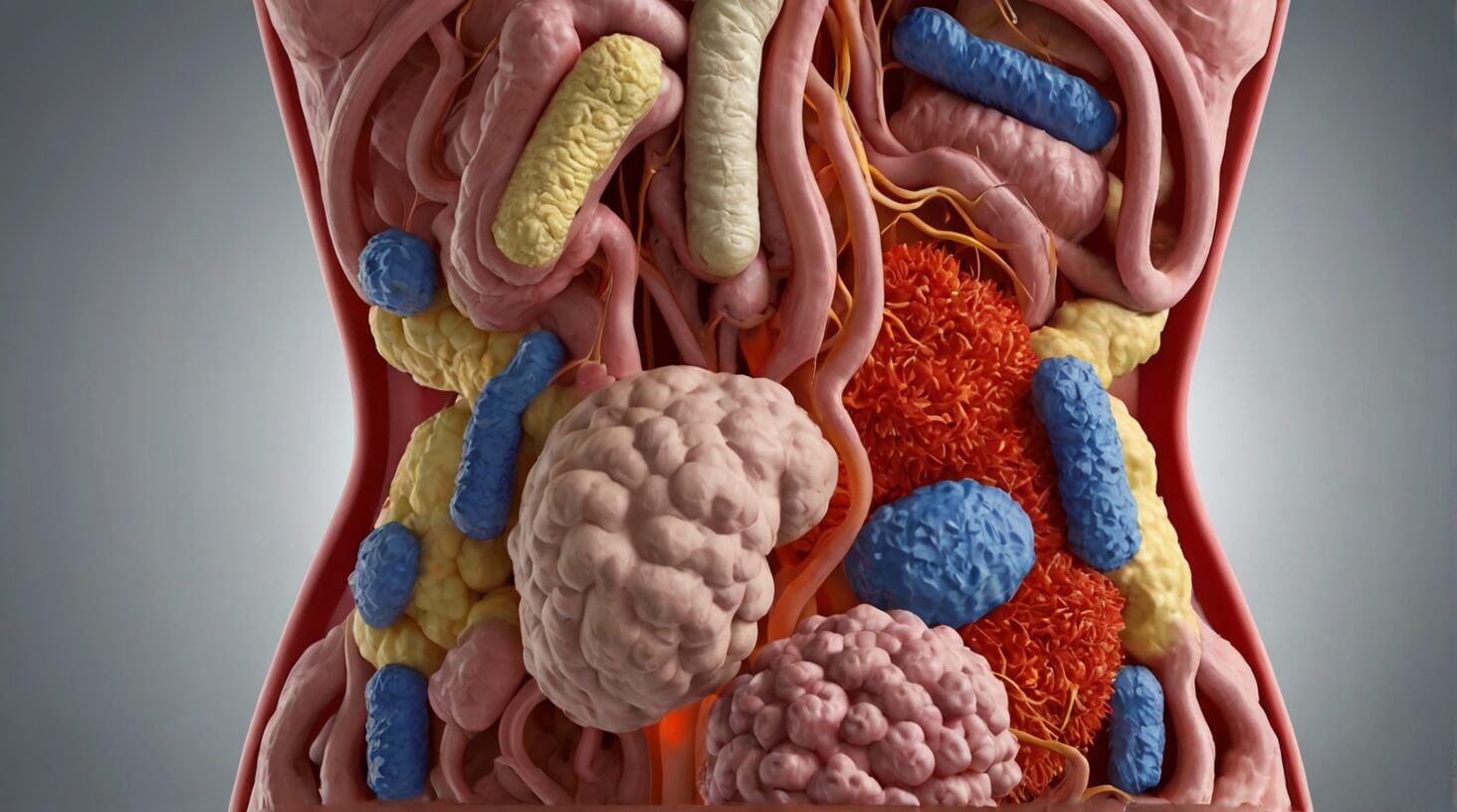
Nearly 70% of your immune system resides within your gut, a fact that highlights the critical importance of gut health in the regulation of inflammation in your body. You may not realize it, but the trillions of microorganisms living in your digestive tract play a pivotal role in your body’s inflammatory response. An imbalance in your gut microbiota, known as dysbiosis, can trigger chronic inflammation, potentially leading to a host of ailments ranging from autoimmune diseases to metabolic disorders. You might be wondering what factors contribute to such an imbalance and how you can modulate your gut environment to favor anti-inflammatory processes. By considering the complex interplay between your diet, lifestyle, and gut health, you can uncover strategies to maintain a balanced gut microbiome, but there’s more to it than just choosing the right foods or taking supplements. Stay with me as we explore the intricate connection between your gut’s health and its impact on inflammation, and consider the emerging evidence that could transform the way you support your overall well-being.
Key Takeaways
- Imbalance in gut microbiota can trigger chronic inflammation, leading to autoimmune diseases and metabolic disorders.
- Manipulating the gut microbiota through probiotics and dietary changes can help reduce inflammation.
- High-fat diets disrupt the balance of gut bacteria and increase inflammation, while fiber-rich and prebiotic-rich diets promote the growth of beneficial gut bacteria.
- Gut flora composition influences levels of inflammatory markers, and specific microbial profiles can influence disease presentations and treatment responses.
Understanding Gut Microbiota

Delving into the intricacies of gut microbiota, it’s essential to understand that this complex community of microorganisms within your digestive tract plays a pivotal role in your health and well-being. The gut microbiota includes a diverse array of bacteria, fungi, parasites, archaea, and viruses, all coexisting in the human gastrointestinal tract. These microorganisms, along with their genetic and functional profiles, constitute the human gut microbiome, which exerts a considerable influence on your health.
You’ll find that humans possess distinct gut microbial compositions, identified as enterotypes. These enterotypes contribute to individual differences in health and the manifestation of diseases. The gut microbiota is instrumental in nutrient absorption, shaping the immune system, and even affecting mental health, thus underscoring its importance in maintaining holistic well-being.
Furthermore, the microbiome’s role in immune system modulation cannot be overstated. It’s a critical player in the development of inflammatory responses. The bacteria in your gut produce short-chain fatty acids (SCFAs) through the fermentation of dietary fibers, which have anti-inflammatory properties and can influence the immune system’s function.
Inflammation is a natural response of the immune system, yet when it becomes chronic, it can lead to various health issues. Targeted manipulation of the gut microbiota through probiotics, prebiotics, and specific dietary changes has shown promise in reducing inflammatory states and improving clinical outcomes. Such therapeutic interventions aim to restore and maintain a balanced microbiome, thereby reducing the risk of inflammation-related diseases. This growing field of research underscores the critical link between gut health and systemic inflammation, offering new avenues for treatment and prevention.
Diet’s Impact on Gut Health
Understanding the role of gut microbiota in immune modulation highlights the importance of examining how your diet influences the health of this microbial community. Your dietary choices have profound effects on gut microbiota, which in turn can modulate metabolic and inflammatory pathways within your body.
Consuming a high-fat diet can disrupt the delicate balance of gut bacteria, often leading to an increase in pro-inflammatory effects. Conversely, a diet rich in fiber, such as one containing legumes, vegetables, fruits, and nuts, can promote the growth of beneficial gut bacteria. These beneficial gut bacteria can help prevent the onset of intestinal inflammatory processes.
To maintain a healthy gut microbiome, it’s essential to focus on foods that either contain or promote the growth of beneficial gut bacteria. Prebiotics, which are found in foods like garlic, onions, and bananas, are a form of dietary fiber that feed good gut bacteria. Probiotic therapies, including fermented foods like yogurt and kefir, introduce beneficial bacteria directly into your gut.
Here’s a brief table to help you visualize the impact of different dietary components on gut health:
| Beneficial Dietary Components | Potential Negative Effects |
|---|---|
| High-fiber foods (legumes, fruits, nuts) | High-fat diets (can lead to dysbiosis) |
| Prebiotic-rich foods (garlic, onions) | Processed foods (often linked to inflammation) |
| Probiotic foods (yogurt, kefir) | Animal-derived foods (may favor harmful bacteria) |
Adopting a diet that supports gut microbiota is crucial for controlling inflammation and maintaining overall health. By choosing the right foods, you’re not just feeding yourself—you’re nourishing the trillions of gut bacteria that play an indispensable role in your well-being.
Gut Microbiota and Immunity
Your gut’s microbiota plays a pivotal role in shaping your immune responses and orchestrating inflammatory processes throughout your body. The diverse collection of microorganisms that reside in your digestive tract, known as gut microbiota, are not mere passengers. They actively engage with your immune system, educating it and influencing its behavior. This interaction primarily occurs at the mucosal surfaces where the majority of your immune cells reside.
The gut microbiota’s influence on the immune system extends to both innate and adaptive immunity, providing crucial signals that can either promote or suppress inflammatory pathways. For instance, certain bacterial species are known to produce short-chain fatty acids that have a role in inhibiting inflammatory reactions and maintaining gut barrier integrity. Conversely, imbalances in microbial composition, often referred to as dysbiosis, can lead to pro-inflammatory effects and contribute to the pathogenesis of inflammatory bowel disease (IBD) and other inflammatory conditions.
It’s essential to understand that microbiota composition differs from person to person, which can explain variations in disease presentations and responses to treatments. Researchers are unraveling how specific microbial profiles can influence the development and severity of diseases characterized by inflammation.
Therapeutic strategies, such as the administration of probiotics and prebiotics or dietary interventions, aim to modulate the gut microbiota to establish a more favorable environment for host health. These interventions can lead to changes in the microbial community that bolster the mucosal immune system and potentially attenuate inflammation, offering promising directions for the management of immune-mediated diseases.
Inflammatory Markers and Gut Flora
The composition of your gut flora significantly influences levels of inflammatory markers, which are pivotal in the regulation of immune responses and the development of various inflammatory conditions. Your gut microbiota, a complex community of microorganisms, plays a crucial role in maintaining health or contributing to disease. Variations in this delicate ecosystem, caused by factors such as diet and genetics, can dramatically alter the production of inflammatory molecules.
Specific species within your gut microbiota produce metabolites that either dampen or exacerbate inflammation. For instance, commensal microbiota often generate short-chain fatty acids with anti-inflammatory properties, promoting a healthier immune system. Conversely, dysbiosis, an imbalance in the gut microbiota, can activate inflammatory pathways involving interleukins and other cytokines, leading to chronic inflammation.
Chronic inflammation is the underlying factor in conditions like inflammatory bowel disease, where dysregulated immune responses to gut microbiota and inflammatory molecules cause damage to the gut lining. Fortunately, modulating the gut microbiota through dietary changes or probiotic interventions can help restore balance, reducing pro-inflammatory effects and improving overall health.
In your efforts to care for others, understanding the connection between gut microbiota and inflammatory markers is essential. By promoting a healthy gut flora, you can influence the immune system to prevent or mitigate inflammatory conditions. Encouraging a diet rich in prebiotics and probiotics, as well as considering individual genetic predispositions, can optimize the gut environment, fostering beneficial microbial communities that support a robust immune response and reduce the risk of chronic inflammation.
Gut Health Linked to Disease
Many chronic diseases, such as obesity, type 2 diabetes, and inflammatory bowel disease, are intricately linked with the health of your gut microbiota. Understanding this connection is critical for devising interventions that could improve patient outcomes. Here are key points that highlight the pivotal role of gut health in disease:
- Dysbiosis and Disease: An imbalance in gut microbiota, known as dysbiosis, has been found to contribute to chronic inflammation and the progression of various diseases.
- Metabolites as Mediators: Some bacteria in your gut can produce metabolites with anti-inflammatory properties, influencing the delicate balance of gut health.
- Microbiota and Chronic Conditions: The complex interplay between gut microbiota and inflammatory molecules is associated with conditions like obesity, atherosclerosis, and type 2 diabetes mellitus.
- Therapeutic Potential: Modifying gut microbiota through diet or microbial interventions may attenuate inflammation and ameliorate disease symptoms.
Your gut microbiota composition differs from others, and these variations can lead to disease and varied responses to treatment. Gut microbiota and inflammation are closely linked, with certain microbes exerting pro-inflammatory effects whilst others may dampen inflammation. Inflammatory pathways that interact with microbiota are triggered by structural components of the bacteria and can cause inflammation in various body systems.
Additionally, the immune system regulation is heavily influenced by the gut microbiota. Inflammatory bowel disease is a prime example where the interplay between microbiota and inflammatory molecules plays a crucial role in the disease’s pathogenesis and clinical course.
Current Research Limitations
Despite significant advances in gut microbiota research, pinpointing exact causal links between microbial patterns and specific diseases remains a formidable challenge. Your clinical acumen is essential in navigating these complexities as you strive to serve your patients effectively.
Recent technological advancements have allowed for better methods of characterising the gut microbiota, yet the composition differs between individuals, which complicates standardization. Longitudinal studies are particularly valuable as they can continually improve our understanding of the various functions influencing gut health over time.
| Research Limitation | Impact on Clinical Practice |
|---|---|
| Lack of causal relationship clarity | Difficulty in prescribing targeted therapy |
| Methodology standardization | Challenges in comparing study results |
| Dynamic microbiota complexity | Uncertainty in long-term patient outcomes |
| Confounding variables influence | Complex patient dietary/lifestyle guidance |
| Microbiota-immune system interactions | Hurdles in developing precise interventions |
You’re tasked with identifying suitable prebiotic and employed in probiotic therapies, yet research doesn’t always highlight relevant knowledge gaps. Understanding reasons behind varying presentations of diseases and how diet, lifestyle, and environmental factors play a role is critical. These limitations impede the development of specific, efficacious interventions.
As a healthcare provider, recognizing these constraints helps you to navigate the current landscape with a detail-oriented and research-based approach. Your dedication to serving others drives the commitment to not only apply existing knowledge but also to advocate for research that delves deeper into the gut microbiota’s influence on inflammation and overall health.
Future Research Directions
Looking forward, it’s crucial for researchers to design studies that can unravel the intricate connections between gut microbiota and systemic inflammation. To guide future research efforts, consider these pivotal areas:
- Advancements in Microbiome Research: Utilize cutting-edge technological advancements to deepen our understanding of the gut microbiota. This includes developing a more refined taxonomic classification system to identify new bacterial species and their roles in health and disease.
- Immune Response Modulation: Investigate how gut microbiota influence immune responses and the production of inflammatory molecules. These studies should aim to elucidate the mechanisms by which the microbiome modulates inflammation both within the gut and throughout the body.
- Development of Probiotic Therapies: Focus on the creation and validation of targeted probiotic therapies. These interventions should be designed based on evidence linking specific strains of beneficial bacteria to the reduction of inflammation in chronic multisystem conditions.
- Integration into Health Research and Implementation: Ensure that findings from gut microbiome research are translated into clinical practice. This involves interdisciplinary collaboration to integrate new discoveries into strategies for disease prevention and management.
As you embark on this journey, remember that inflammation underlies many chronic multisystem conditions, making this line of inquiry not only intellectually compelling but also deeply relevant to patient care. Your work has the potential to transform lives by contributing to the development of novel diagnostic and therapeutic strategies that serve the greater good. Stay detail-oriented and committed to excellence as you contribute to this vital area of health research and implementation.