Have you ever considered how the pain and redness of a stubbed toe are actually signs of your body’s sophisticated defense system at work? As you navigate the complexities of health, it’s essential to understand that inflammation is your body’s innate response to protect and heal itself. While you often hear about the negative consequences of chronic inflammation, it’s the balance between inflammation and anti-inflammatory mechanisms that keeps you healthy. You’re aware of the critical role lifestyle choices play in tipping this balance, but what if there’s more to the story? Imagine uncovering the fine line between necessary immune response and the pathway to chronic illness, and the power such knowledge could grant you in taking control of your health. Let’s explore the fundamental dynamics of inflammation and how it can be both a friend and foe, setting the stage for a deeper insight into the silent battles raging within your body.
Key Takeaways
- Inflammation is a natural response to injury and infection, but chronic inflammation can contribute to chronic diseases like heart disease and diabetes.
- Acute inflammation is a protective and localized response to injury or infection, while chronic inflammation is a prolonged, systemic assault on the body’s own tissues.
- Chronic inflammation can lead to diseases such as rheumatoid arthritis, cancer, atherosclerosis, heart disease, diabetes, and asthma.
- Management strategies for chronic inflammation include medication, lifestyle changes, targeted therapy, anti-inflammatory diets, statin therapy, glucose management, and avoiding triggers.
The Fundamentals of Inflammation

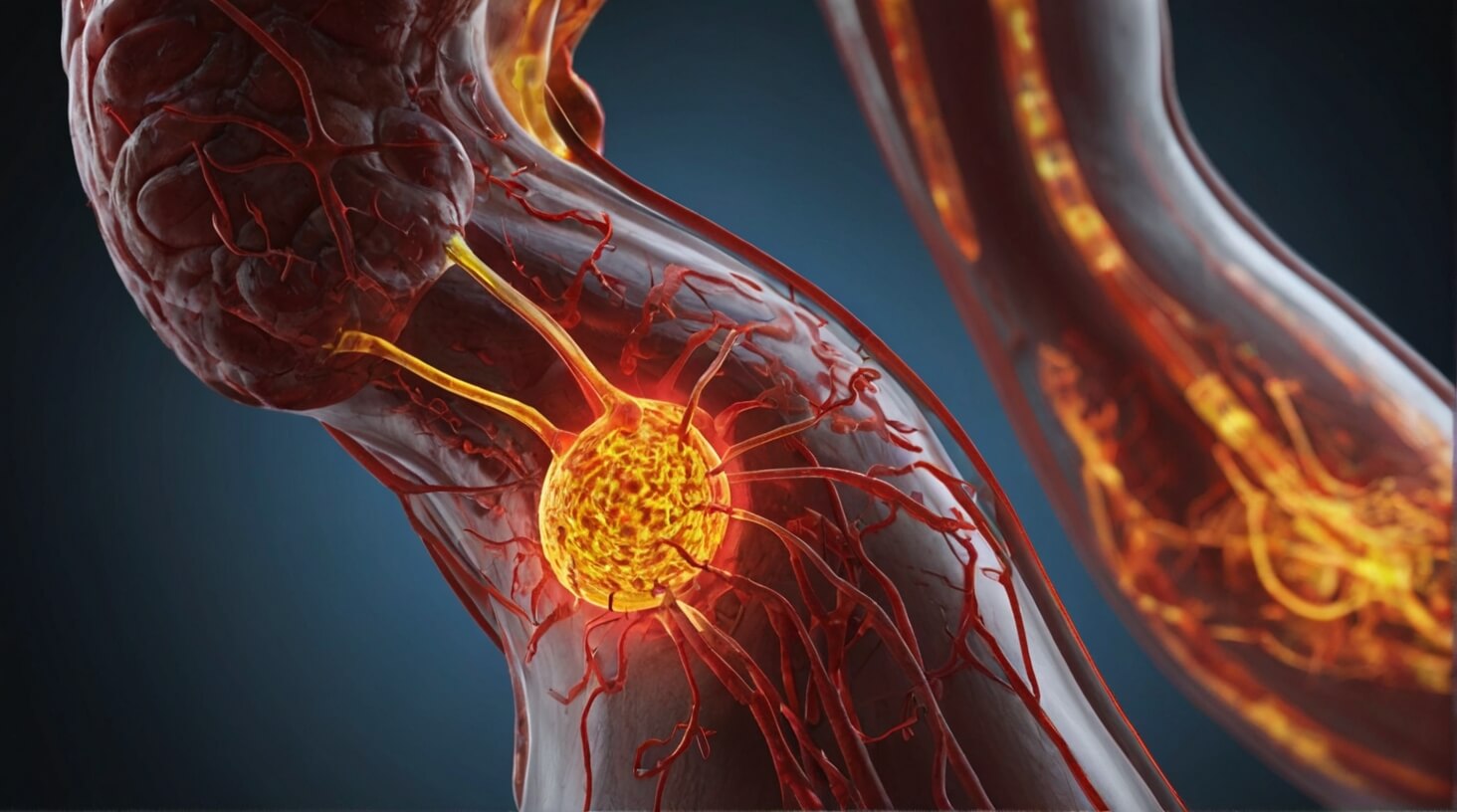
Understanding the basics of inflammation is crucial, as it’s not only a fundamental biological response to injury and infection but also a double-edged sword that, when uncontrolled, can contribute to a myriad of chronic diseases. You must recognize that inflammation is essential for the healing process. Your body’s immune system responds to tissue damage by initiating an inflammatory response, which is characterized by redness, heat, swelling, and pain at the affected site. This is known as acute inflammation.
Acute inflammation helps fight off infections by attracting immune cells to the site of injury, thereby speeding up the healing process. However, when inflammation persists and becomes less about immediate response and more about long-term presence, it morphs into chronic inflammation. Chronic inflammation plays a detrimental role in the body, often silently contributing to the progression of diseases such as heart disease, diabetes, and cancer.
It’s imperative to understand that your lifestyle choices have a significant impact on your body’s inflammatory response. Certain foods, for instance, can either promote or inhibit inflammation. A diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can help keep inflammation at bay, while processed foods and sugars may exacerbate it.
Moreover, regular medical check-ups are a proactive measure to detect chronic inflammation. Such vigilance can help you identify and address potential underlying conditions before they escalate. As someone dedicated to serving others, appreciating the nuanced roles of acute and chronic inflammation ensures that you can provide informed care, guiding those you serve towards maintaining a balanced immune response and overall better health.
Acute Vs. Chronic Inflammation
Delving into the dichotomy of acute versus chronic inflammation reveals a pivotal difference: acute inflammation serves as a protective and localized response to injury or infection, while chronic inflammation represents a prolonged, often systemic assault on the body’s own tissues. When you’re faced with a response to an injury, such as a cut or a sprain, your body’s white blood cells rush to the scene. This acute phase is characterized by classic signs: redness, warmth, swelling, and pain. These symptoms are actually signs that your body is working hard to heal.
On the other hand, chronic inflammation is a more insidious condition. It occurs when this inflammatory response doesn’t shut off as it should, leading to your immune system mistakenly attacking healthy tissues. Over time, this persistent state of inflammation can contribute to a host of diseases, including arthritis, diabetes, and heart disease.
To grasp the complexities of inflammation’s impact on health, consider the following points:
- Acute Inflammation: Quick and localized, it’s essential for healing. White blood cells play a crucial role by engulfing pathogens and kickstarting the healing process.
- Chronic Inflammation: A slow-burning fire within your body that can erode health over time. The role that chronic inflammation plays in various diseases highlights the importance of identifying and managing it early.
- Management Strategies: For acute inflammation, simple measures like cold compresses and over-the-counter pain relief are often sufficient. Chronic inflammation, however, demands a multifaceted approach including medication, lifestyle changes, and dietary adjustments.
Inflammation is involved in many aspects of health and disease. As someone dedicated to serving others, understanding the nuances between acute and chronic inflammation is vital for fostering health and wellbeing in those you care for.
Inflammation’s Impact on Diseases

Recognizing the contrast between acute and chronic inflammation, it’s crucial to explore how the latter’s persistence contributes to a spectrum of diseases, including but not limited to rheumatoid arthritis, cancer, and heart disease. Chronic inflammation acts as a nefarious agent in the body, insidiously promoting the development and progression of these conditions. You, as a healthcare provider, must understand that chronic inflammation isn’t merely a reaction but a contributing factor that can exacerbate and even initiate disease processes.
When you’re dealing with inflammatory conditions, it’s important to recognize that chronic inflammation plays a role in the pathology of diseases like rheumatoid arthritis. This autoimmune disorder is characterized by prolonged inflammation leading to joint damage and systemic complications. Similarly, inflammation is implicated in the onset and progression of certain cancers, where it can promote tumor growth and metastasis.
In the context of cardiovascular disease, chronic inflammation contributes to atherosclerosis, a condition where plaque builds up in the arteries, which can lead to heart disease. It’s evident that inflammation’s role is not just secondary but central to the pathology of these diseases.
Here’s a table to illustrate the impact of chronic inflammation on various diseases:
| Disease | Impact of Chronic Inflammation | Management Strategies |
|---|---|---|
| Rheumatoid Arthritis | Joint damage, systemic issues | Anti-inflammatory meds, lifestyle changes |
| Certain Cancers | Tumor promotion, metastasis | Targeted therapy, anti-inflammatory diet |
| Heart Disease | Atherosclerosis, plaque buildup | Lifestyle changes, statin therapy |
| Diabetes | Insulin resistance, beta-cell dysfunction | Dietary adjustments, glucose management |
| Asthma | Airway hyperresponsiveness | Steroids, avoiding triggers |
You must approach these health challenges with a detailed understanding, advocating for preventative measures and targeted treatments to mitigate the harmful effects of chronic inflammation on your patients’ well-being.
Managing Chronic Inflammation
To effectively manage chronic inflammation, you must integrate a multifaceted approach that includes pharmacological interventions, dietary modifications, and lifestyle adjustments tailored to individual patient needs. Chronic inflammation can increase the risk of numerous diseases and conditions, underscoring the need for a strategic management plan to help protect the body’s tissues and organs.
Here are three pivotal elements to consider when managing chronic inflammation:
- Pharmacological Interventions: These may involve nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or disease-modifying antirheumatic drugs (DMARDs). These medications can reduce inflammation and alleviate pain. However, the selection of appropriate medication must be personalized, considering potential side effects and the specific inflammatory pathways involved in the patient’s condition.
- Dietary Modifications: A diet rich in anti-inflammatory foods such as fruits, vegetables, nuts, fatty fish, and whole grains can support the management of chronic inflammation. Conversely, a diet high in processed foods, trans fats, and sugar can exacerbate inflammation. Nutritional interventions should aim to provide a balanced intake of antioxidants and omega-3 fatty acids, which have been shown to reduce inflammatory biomarkers.
- Lifestyle Adjustments: Regular physical activity, stress reduction techniques, and adequate sleep are crucial in managing chronic inflammation. Exercise can decrease pro-inflammatory cytokines and promote the release of anti-inflammatory substances. Mind-body practices like meditation and yoga can help modulate the stress response, which is known to contribute to inflammation. Ensuring sufficient restorative sleep is also essential, as sleep disturbances can exacerbate inflammatory processes.
Each patient’s journey in managing chronic inflammation is unique, and interventions should be adapted to their individual health profiles and the specific etiology of their inflammatory state.
Strategies for Reducing Inflammation

Implementing an anti-inflammatory lifestyle involves strategic dietary choices, regular physical activity, and stress management techniques to mitigate the adverse effects of chronic inflammation. You’ll need to delve deep into the scientific intricacies of Understanding Inflammation to tailor a comprehensive plan that addresses this pervasive health challenge.
Begin by reevaluating your intake of refined carbs, which have been linked to an increase in inflammation. Studies suggest that these foods can cause a spike in blood sugar, leading to an overproduction of pro-inflammatory cytokines. Instead, you should focus on consuming a balanced diet rich in whole foods that contain anti-inflammatory compounds. Foods such as fatty fish, rich in omega-3 fatty acids, and leafy greens, high in antioxidants, play a critical role in modulating the body’s inflammatory response.
Physical activity, too, is a cornerstone of reducing inflammation. Regular exercise promotes the release of anti-inflammatory cytokines, which can help reduce the redness and swelling often associated with inflammation. It’s not just about the intensity but also the consistency of your exercise regimen that contributes to long-term anti-inflammatory benefits.
Stress management is another key strategy. Chronic stress is a known contributor to inflammation, as it triggers the release of stress hormones that can exacerbate the body’s healing process. Techniques such as mindfulness, yoga, and deep-breathing exercises are effective in reducing stress-related inflammation.
As you serve your community, it’s vital to communicate that combating inflammation isn’t a one-off effort but a persistent commitment to a lifestyle that values the role of holistic health practices. With this approach, you empower others to take proactive steps in managing their well-being.