Have you ever wondered if the ancient practice of acupuncture truly has the power to enhance your immune system? You’re not alone in this curiosity. As you navigate through your busy life, your body’s immune response silently works as your personal defense mechanism, but sometimes it needs a boost. Acupuncture, with its roots deeply embedded in traditional Chinese medicine, has long been touted for its health benefits—among them, the purported ability to modulate immune function. Professional studies hint at its potential to not only prevent illness but also to play a significant role in treating immune-related conditions. While skeptics may question its efficacy, emerging research suggests there’s more to this needle-based therapy than mere placebo effect. The real question is, how does something as simple as strategically placed needles influence complex immune responses? Keep exploring, and you just might find the intersection of ancient wisdom and modern science more intriguing than you expected.
Key Takeaways
- Acupuncture regulates the immune system and maintains overall immune balance.
- Acupuncture enhances innate immunity, the body’s first line of defense against pathogens.
- Acupuncture modulates the adaptive immune response, crucial for long-term immunity.
- Acupuncture influences neuroimmune connections, critical for immune responses and neurological functions.
Understanding Immune Response
Your body’s immune system is a complex network that, while designed to shield you from infections and diseases, can sometimes become overactive, leading to conditions such as allergies and autoimmune disorders. A properly functioning immune response is crucial for maintaining health, yet when dysregulated, it may inadvertently attack the body’s own tissues or respond excessively to harmless stimuli.
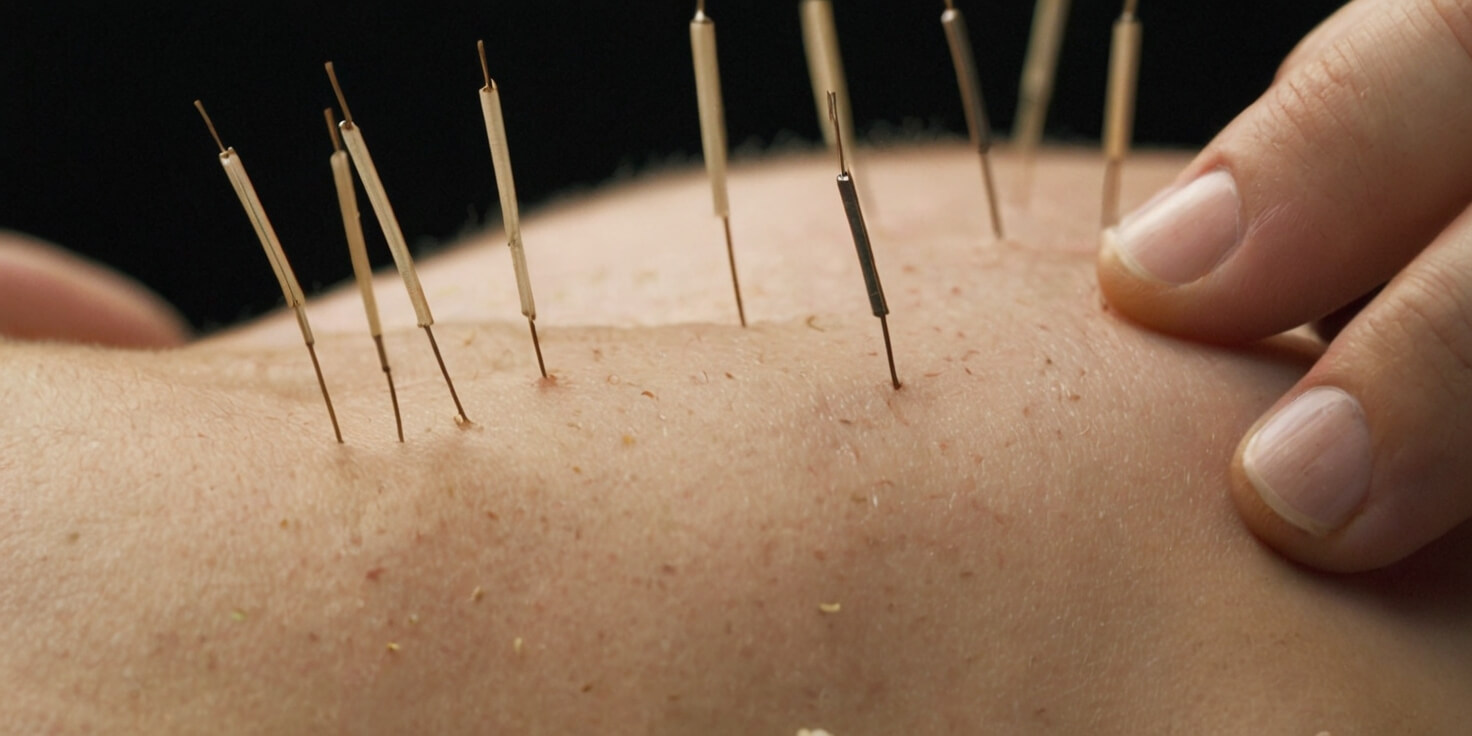
Acupuncture, an ancient Chinese medical practice, has been shown to regulate the immune system. This regulation is critical, as it contributes to disease prevention and treatment by maintaining overall immune balance. It employs a mechanism of acupuncture that involves the insertion of fine needles into specific points on the body to stimulate the body’s natural defense mechanisms. This stimulation can enhance the immune system’s ability to combat pathogens, including cold viruses and influenza.
Recent scientific research supports the efficacy of acupuncture in enhancing anticancer and antistress immune functions while exerting anti-inflammatory effects. Through its ability to modulate the immune response, acupuncture serves as a therapeutic ally in managing chronic health conditions. It also provides relief from acute pain and discomfort, thereby reducing stress and anxiety levels, which are known to compromise immune function.
As someone dedicated to serving others, understanding and leveraging acupuncture’s potential to harmonize the immune response is paramount. By applying this knowledge, you can aid individuals in achieving a state of health where their immune systems operate efficiently without being overactive or suppressed, thus fostering resilience against a range of health challenges.
Acupuncture and Innate Immunity
Building on the understanding of immune system regulation, let’s explore how acupuncture specifically bolsters innate immunity, the body’s first line of defense against pathogens. Acupuncture, a traditional Chinese medicine practice, has garnered attention for its capacity to enhance the immune system’s function in defense, homeostasis, and surveillance. It is now understood that acupuncture can regulate the immune system in a way that notably benefits innate immunity.
Research indicates that acupuncture’s influence extends to regulating immune cells, which are pivotal to the innate immune response. These cells, including macrophages, neutrophils, and natural killer cells, act swiftly to combat foreign invaders. By stimulating specific points on the body, like the widely used ST36 (Zusanli), acupuncture can potentially modulate the activity and efficacy of these cells, thereby enhancing your body’s natural immune response.
Moreover, acupuncture’s anti-inflammatory effects are critical, as inflammation is a common response of the innate immune system to harmful stimuli. Inflammation, while protective, can become chronic and detrimental if not well-regulated. Acupuncture’s ability to modulate this response makes it a valuable ally in preventing and treating various immune-related diseases, including conditions like Crohn’s disease, where moxibustion combined with acupuncture shows potential for clinical application.
As acupuncture integrates into Western medical practices, its role in supporting and regulating the immune system, particularly innate immunity, becomes increasingly evident. For those dedicated to serving others through healthcare, understanding and utilizing acupuncture’s capacity to harmonize immune function could greatly enhance patient care and outcomes in immune-related conditions.
Modulating Adaptive Immunity
While acupuncture is well-known for its role in pain relief, it also significantly modulates the adaptive immune response, a complex system crucial for long-term immunity and immunological memory. Research has shown that this traditional practice can enhance survival rates in conditions like sepsis by tapping into adaptive immunity pathways. Its efficacy in treating inflammatory conditions, such as inflammatory bowel syndrome, highlights acupuncture’s potential to regulate inflammation-related cytokines and immune cell differentiation, which are pivotal in adaptive immunity.
Acupuncture’s anti-inflammatory role is particularly evident in asthma, where it influences the number and activity of CD4 T cells. By enhancing Th1 cell activities and bolstering regulatory T (Treg) cell functions, acupuncture helps create a more balanced immune response in asthma models. This fine-tuning of the immune system is not solely limited to helper T cells; acupuncture can also regulate the differentiation of CD8 T cells and adjust the ratio of various lymphocyte subsets, further evidencing its capacity to modulate adaptive immunity.
Moreover, acupuncture’s impact extends to natural killer (NK) cells, a bridge between innate and adaptive immunity. By modulating the quantity and activity of NK cells, acupuncture boosts their cytotoxic activity and promotes the release of cytokines, contributing to an array of immunosuppressive effects.
In your role as a healthcare provider, understanding acupuncture’s ability to modulate adaptive immunity is invaluable. It’s a tool that can be integrated into patient care strategies, enhancing their immune response and potentially improving clinical outcomes for a variety of immune-related conditions.
Acupuncture’s Neuroimmune Connections

Having explored how acupuncture modulates adaptive immunity, let’s now examine its influence on neuroimmune connections, which are critical in both immune responses and neurological functions. The neuroimmune system is a complex network where the nervous and immune systems communicate and influence one another. Acupuncture acts as a mediator in this dialogue, often promoting immune balance and contributing to the body’s natural healing processes.
One of the ways acupuncture exerts its effects is by engaging the cholinergic anti-inflammatory pathway. This pathway is a prime example of the neuroimmune interface, where the nervous system can regulate immune responses and inflammation. Stimulating specific acupuncture points can activate this pathway, leading to reduced inflammation and improved immune function.
To understand the breadth of acupuncture’s impact on neuroimmune connections, consider the following points:
- Regulation of Immunity: Acupuncture can enhance antistress and anticancer immune functions, aiding the body’s resilience.
- Protection of Intestinal Mucosa: The ST36 acupuncture point is associated with the protection of the intestinal mucosal immune barrier, crucial in septic conditions.
- Balance of Th17/Treg Cells: Treatments like moxibustion and acupuncture can influence the balance between Th17 and Treg cells, which is vital for managing autoimmune diseases like Crohn’s.
- TLR2/NF-κB Signaling: Herb-partitioned moxibustion has been shown to regulate this signaling pathway, promoting repair in ulcerative colitis.
- Anti-Inflammatory Effects: Acupuncture demonstrates a capacity to alleviate inflammation and hyperalgesia, indicating its role in immune modulation.
In your work to serve others through holistic healthcare, it’s essential to recognize the scientific basis for acupuncture’s benefits, particularly its ability to facilitate neuroimmune communication and foster immune equilibrium.
Hormonal Pathways and Immunoregulation
Acupuncture frequently modulates hormonal pathways, playing a pivotal role in the immunoregulatory processes that maintain health and combat disease. By engaging specific points on the body, this ancient practice not only influences the neuroendocrine system but also intersects with complex immunoregulation mechanisms. Scientific studies have shown that acupuncture can enhance anticancer and antistress immune functions, underscoring its potential as a complementary therapy in various health conditions.
Electroacupuncture, particularly at the ST36 point, has been found to protect the intestinal mucosal immune barrier during sepsis, a critical state where the body’s response to infection can lead to tissue damage, organ failure, or death. You’ll find this intervention is especially relevant in clinical settings where sepsis is a concern.
Furthermore, therapies such as moxibustion and acupuncture have demonstrated efficacy in ameliorating Crohn’s disease. They achieve this by regulating the delicate balance between Th17 cells, which are pro-inflammatory, and Treg cells, which promote immunological tolerance. This balance is crucial for the health of the intestinal mucosa and the overall immune response.
Herb-partitioned moxibustion takes this a step further by regulating the TLR2/NF-κB signaling pathway, which is involved in the inflammatory response associated with ulcerative colitis. Through this modulation, the therapy promotes the repair of the damaged colonic mucosa, offering a beacon of hope for patients suffering from this debilitating condition.
Lastly, acupuncture’s anti-inflammatory effects are not limited to local areas of treatment. They also activate a novel cholinergic anti-inflammatory pathway, which could revolutionize how we approach conditions characterized by systemic inflammation. As you incorporate these therapies into your practice, bear in mind that your goal is to harness these pathways to optimize immunoregulation and enhance patient outcomes.
Clinical Studies on Acupuncture Efficacy
Building on the immunomodulatory effects discussed, let’s examine the clinical evidence supporting acupuncture’s efficacy in treating various health conditions. Research on acupuncture, which includes randomized controlled trials, points toward its potential benefits across a spectrum of immune-related diseases.
Clinical studies on acupuncture efficacy have shown that the technique can regulate immunity. For instance, acupuncture point ST36 (Zusanli) is particularly noted for its role in improving immune cell concentration and percentages, which is critical in the management of immune-related conditions. Furthermore, the combination of moxibustion and acupuncture has been found effective in treating inflammatory diseases such as Crohn’s disease. This is achieved through the regulation of immune cell types, specifically the balance between Th17 and Treg cells within the intestinal mucosa.
The anti-inflammatory effects of acupuncture are also well-documented. It can alleviate inflammation and hyperalgesia by activating mediators and signaling pathways, which is pivotal in treating a variety of inflammatory conditions. Here are some key findings from recent studies:
- Regulation of immunity, enhancing anticancer and antistress immune functions.
- Improvement in immune cell concentration and percentage via ST36.
- Effectiveness in treating Crohn’s disease by regulating Th17 and Treg cell balance.
- Potential in treating ulcerative colitis by modulating TLR2/NF-κB signaling pathways.
- Alleviation of inflammation and hyperalgesia through various mediators and signaling pathways.
These points underscore the scientific basis for the use of acupuncture in clinical settings. As you serve others with this knowledge, it is important to rely on up-to-date and rigorously validated research to ensure the best outcomes for patients seeking alternative or complementary therapies.
Lifestyle Integration and Immune Health

Integrating acupuncture into your lifestyle can significantly bolster your immune system’s resilience and efficiency. As you seek to serve others, it’s crucial to understand that a healthy immune system is the cornerstone of maintaining overall health. The deliberate inclusion of acupuncture practice into daily routines can have profound effects on immune health. Scientific research suggests that lifestyle integration of regular acupuncture sessions can regulate immune function, increasing the production of immune cells and enhancing the body’s natural defense mechanisms against pathogens.
Acupuncture’s role in stress reduction is well-documented. By promoting relaxation and improving sleep quality, acupuncture has the potential to create a more conducive environment for immune health. Stress is a known immune suppressor; therefore, reducing its levels through acupuncture can lead to more robust immune responses and reduced susceptibility to illnesses.
Furthermore, acupuncture provides relief for chronic conditions, which can be particularly taxing on the immune system. By supporting overall well-being and complementing conventional medical treatments, acupuncture practice offers a holistic approach to healthcare. This holistic perspective not only addresses the immediate symptoms but also targets underlying issues that may compromise the immune system.
The effectiveness of acupuncture in fostering a healthy immune system is not just temporary. When integrated into one’s lifestyle, it can lead to long-lasting remedies and improved function of the immune system. It’s important to appreciate that such integration is a commitment to one’s health that can yield dividends in the form of reduced illness frequency and improved quality of life for those who consistently follow through with this ancient, yet scientifically supported, healthcare practice.











