Autoinflammatory disorders (AIDs) are rare and complex conditions. They happen when the body’s immune system becomes too active. If you or someone you care about has AIDs, it’s essential to know about the causes, symptoms, diagnosis, and treatments.
This article will explain AIDs in simple terms and tell you how to manage them. We’ll look at why the immune system acts up and how researchers are studying AIDs for better treatments. Knowing this information will help you make better decisions when caring for yourself or someone you love.
Definition of Autoinflammatory Disorders
Autoinflammatory disorders are rare conditions caused by changes in the body’s proteins. These make the immune system trigger inflammation even without an infection. Genetic mutations can cause these changes either through inheritance or during early development. Sometimes, infections or trauma can trigger symptoms.
The most common type is Familial Mediterranean Fever (FMF). This affects people from certain regions and causes fever, abdominal pain, joint pain, and rashes. Other types like CAPS, HIDS, TRAPS, Blau Syndrome, and Majeed Syndrome can start at a young age or any age.
The severity of autoinflammatory conditions can vary, and they need different treatments. Medications like nonsteroidal anti-inflammatories or steroids can help. But more severe cases may need biological agents like interferon alpha or anakinra. Lifestyle changes, nutrition, and physical activity can improve the lives of those with these diseases.
Causes and Risk Factors of AIDs
Ignoring the risks of AIDS can be dangerous – it’s like playing with fire! HIV (Human Immunodeficiency Virus) is a virus that attacks the immune system. If not treated, it can lead to AIDS (Acquired Immune Deficiency Syndrome). People who are more likely to get HIV are those who use drugs with needles and have sex without protection with many different partners. Even those who touch infected blood or needles. People with high HIV infection rates in their birthplaces may as well have a higher chance of exposure.
To prevent AIDS, you should avoid risky behaviors like unprotected sex and sharing needles. If you do have sex, use condoms to protect yourself. Get tested to catch any signs of AIDS early, so you can get the right treatment as soon as possible.
Knowing the signs and symptoms of AIDS is important for early diagnosis and treatment. Symptoms may include frequent fevers, swollen lymph nodes, weight loss, or feeling tired. If you think you might have exposure to HIV or another autoinflammatory disorder, talk to your doctor or get medical help right away. Taking care of your health will help you live a long, healthy life without disease.
Symptoms of Autoinflammatory Disorders
Knowing the signs and symptoms of autoinflammatory disorders can help you stay healthy and take care of yourself. These conditions happen when the innate immune system in your body doesn’t work right. This is because of things like genetic mutations, infections, or environmental factors. Symptoms vary depending on the type of disorder but generally include:
- Fever: Often recurrent and prolonged episodes of fever lasting several days
- Pain: Joint pain, abdominal pain, chest pain, or headaches
- Rash/Skin Issues: Rashes, hives, or other skin issues
- Swelling/Swelling: Swelling in various areas such as eyes, face, or joints
- Fatigue: Extreme tiredness often accompanied by general malaise
Autoinflammatory disorders have accompanying symptoms like loss of appetite, weight loss, and anemia. Sometimes, patients may feel depressed or anxious due to their condition. Doctors diagnose these disorders based on medical history and lab tests to find the cause. Early diagnosis is important for successful management. So it’s crucial to seek medical attention if any symptoms appear. By being aware of potential signs and symptoms, you can address any issues easier.
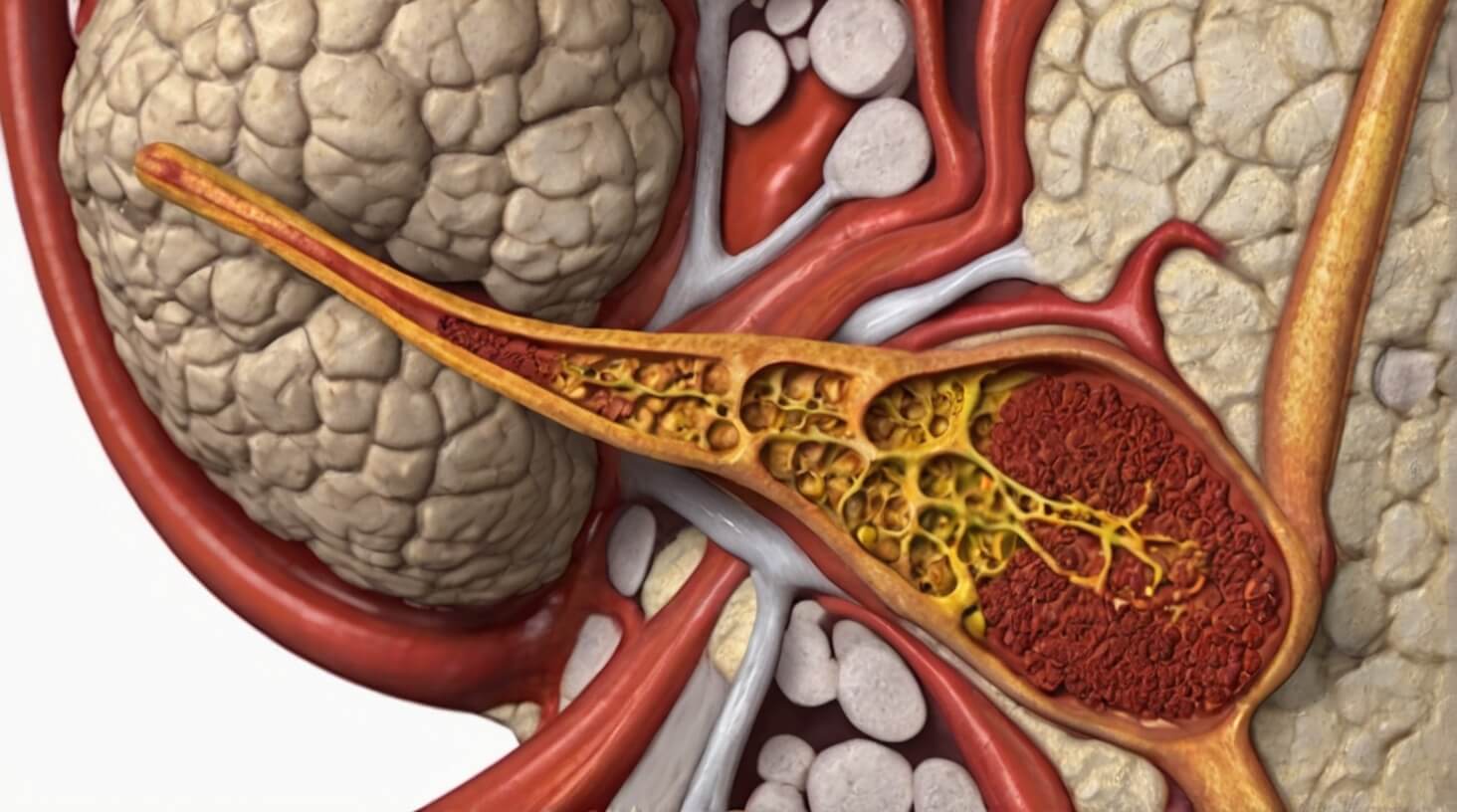
Diagnosing Autoinflammatory Disorders

If you think you have an autoinflammatory disorder and have severe symptoms, it’s crucial to get a diagnosis right away. Diagnosing these disorders can be hard, so doctors will use genetic testing and medical history to find out for sure. Doctors might use tests to find out if genetic mutations are causing autoinflammatory disorders. Examples of these are whole exome sequencing or gene panel testing. After these tests, the doctor might do more lab tests to confirm their suspicions and rule out other conditions with similar symptoms.
Doctors will do physical exams to check for signs of inflammation in the eyes, skin, joints, and other parts of the body. They may ask about your family’s medical history since some autoinflammatory disorders run in families. By gathering all this information, the doctor can make the right diagnosis.
It’s important to stay informed during the diagnostic process and work with your doctor to get the best care for your condition. With the right identification and treatment plans made only for you, you can find relief from your symptoms and have a healthier life ahead.
The Innate Immune System and Dysregulation
When our body’s innate immune system is not working the proper way, it can cause autoinflammatory disorders. This system helps protect us from infections and foreign things. It uses inflammation to activate cells and molecules that fight off these invaders.
Sometimes, due to genetic or environmental factors, this process can go wrong. When that happens, it can lead to diseases. Such as systemic juvenile idiopathic arthritis (SJIA) or familial Mediterranean fever (FMF).
In these conditions, the body doesn’t recognize the harmful agents. This causes long-lasting and uncontrolled inflammation. This leads to chronic inflammation and damage to tissues over time. To understand these diseases better, we need to know how the innate immune system works and what happens when it doesn’t work the proper way.
Treating autoinflammatory disorders can involve blocking certain inflammatory molecules with medications. One way is through anti-interleukin treatments. Other options include biologics, steroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and more. These treatments help control the inflammation and manage the symptoms.
- Identifying potential triggers for flare-ups
- Monitoring symptoms with healthcare providers
- Taking prescribed medication as directed
- Making lifestyle changes like exercise and stress management * Eating a healthy diet that is low in inflammatory foods.
Current Research and Treatments
Researchers are studying autoinflammatory disorders to find better treatments. They are looking at genetic factors and lifestyle changes to help reduce symptoms and prevent the disorders. Some research has shown promising results for potential treatments.
They are looking into what might trigger the disorders and what causes infection and toxins. This can help understand why some people get these disorders and how lifestyle changes might help prevent them. Diet changes could be a way to reduce inflammation in people who already have an autoinflammatory disorder.
Researchers are testing medications in clinical trials to treat these disorders. Some drugs target specific inflammatory pathways, and others suppress inflammation throughout the body. While these medicines can’t cure the condition, they can help ease symptoms and make life better for patients.
Long-Term Outlook for AIDs

Having an autoinflammatory disorder can be tough, and the future is uncertain. But there is hope because of research and treatments.
New drugs are helping to control symptoms, but a cure isn’t found yet. Autoinflammatory disorders happen because of genetic mutations. They mess up the immune system, causing chronic inflammation and other problems.
People with these disorders might have to live with them for a long time. But managing symptoms is vital for a good quality of life.
Doctors need to keep track of the disease and adjust treatments as needed. Some drugs might have side effects, and it varies from person to person.
Diagnosing and treating autoinflammatory disorders are complex things to do. But, many patients say personalized treatment plans make them feel better.
Researchers are learning more about the genetics of AIDs, and it could lead to better treatments in the future.
Living with AIDs means long-term management, but with the right care and information, people can have better lives. More research and awareness campaigns give hope for improved treatments in the future.
Frequent-Asked Questions
What lifestyle changes can I make to reduce my risk of developing an autoinflammatory disorder?
Staying healthy and reducing the risk of autoinflammatory disorders is important. You can do this by eating a balanced diet with lots of vitamins and minerals. Getting enough sleep, avoiding smoking and excessive drinking, and being active every day are good for your health. Managing stress through yoga or meditation can help too. Remember to take care of yourself to stay well!
How can I tell if I have an autoinflammatory disorder?
If you think you might have an autoinflammatory disorder, watch out for common signs like fever, rash, joint pain, and swollen lymph nodes. It can be hard to diagnose without genetic testing, so talk to your doctor if you notice recurring inflammation. They can help you figure out what to do and manage any symptoms you have. Rest and pain relief medications can help too. If you’re worried about your risk, talk to your doctor to decide the best plan for you.
Are there any natural remedies for autoinflammatory disorders?
You may have heard of autoinflammatory disorders, but did you know that there are natural remedies for treating them? Dietary changes and stress management can both be effective ways to manage symptoms. Start by focusing on adding anti-inflammatory foods, such as fatty fish, nuts and seeds, berries, and leafy greens to your diet. This helps balance out any inflammatory responses in the body. Additionally, managing stress can help reduce inflammation as well. You may find yoga or meditation helpful in this regard or even look into activities like journaling or deep breathing exercises. With a little bit of effort each day, you can make a real difference in how your autoinflammatory disorder affects you in the long run.
What are the potential long-term effects of autoinflammatory disorders?
It’s important to know about autoinflammatory disorders and their effects. If not treated, they can cause many problems like pain, fatigue, and less physical ability. They can increase the risk of infection and damage to organs. People with these disorders may also have mental health issues like depression and anxiety. So, it’s essential to get medical help early to avoid these long-term effects.
Are there any new treatments or research in development for autoinflammatory disorders?
Scientists are working on new treatments for autoinflammatory disorders. They are looking at specific therapies that target the disorder’s genetic causes. These therapies focus on certain triggers that cause inflammation in the body. Researchers are studying ways to reduce inflammation using medications like corticosteroids and NSAIDs. They are even exploring treatments like gene therapy and cell transplantation. The goal is to find ways to reduce symptoms, slow down the disease, and even cure it completely.
You’ve learned a lot about how changes in certain genes cause autoinflammatory disorders. AIDs can have signs and symptoms that you need to watch out for. Doctors can diagnose and treat these diseases.
More research is necessary to improve treatments and help people with autoinflammatory disorders. With hard work, we can provide better care for them and help them lead more normal lives, like a butterfly emerging from its cocoon.