Congratulations, you’ve just been handed the keys to one of your body’s most paradoxical features: inflammation, the silent guardian and the occasional betrayer. As you navigate through your daily life, your body’s inflammatory response is constantly on the lookout for trouble, ready to leap into action at the first sign of invasion or injury. It’s a finely tuned system that protects, repairs, and sometimes, regrettably, overreacts. You might not give much thought to the complex interplay of cells, chemicals, and signals that swirl into motion to shield you from harm, yet this process is central to your well-being. But what happens when this protector turns into a perpetrator, contributing to a range of chronic diseases? Stay with me, and you’ll uncover the mechanisms that govern this double-edged sword of health and how understanding them could be the secret to keeping it sharp when you need it and sheathed when you don’t.
Key Takeaways
- Inflammation is a complex biological response aimed at removing harmful substances and initiating healing.
- There are two types of inflammation: acute and chronic. Acute inflammation is immediate and necessary, while chronic inflammation is prolonged and can lead to tissue and organ deterioration.
- Symptoms of inflammation include redness, heat, swelling, and pain. Chronic inflammation can cause persistent joint pain, skin rashes, and abdominal discomfort.
- Understanding inflammation is important for precise diagnosis, tailored interventions, and early intervention to prevent the progression of chronic inflammatory diseases.
Defining Inflammation
Inflammation is your body’s complex biological response to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective mechanism aimed at removing these detrimental substances and initiating the healing process. As an integral component of the immune system, inflammation recruits immune cells to the affected tissue, orchestrating a series of events that serve to isolate and eradicate the offending agents.
When you sustain an injury or encounter an infection, your body’s defense system triggers an acute inflammatory response. This response is characterized by the rapid mobilization of inflammatory cells, including leukocytes, to the site of injury. These immune cells release cytokines and other mediators that cause the classic signs of inflammation: redness, heat, swelling, and pain. These symptoms, while often uncomfortable, are indicative of your body’s healing processes at work.
Conversely, chronic inflammation arises when the immune response does not cease appropriately. Instead, inflammatory cells persist, sometimes even in the absence of an external threat, potentially leading to a state of continuous immune system activation. Over time, this can inflict damage on tissues and organs, manifesting in various chronic diseases such as rheumatoid arthritis, heart disease, and type 2 diabetes.
Understanding the distinction between acute and chronic inflammation is crucial for those who aim to serve others in the medical and health fields. It allows for precise diagnosis and tailored interventions to ameliorate inflammatory conditions. Recognizing the signs and contributing factors to chronic inflammation, such as autoimmune disorders and persistent acute inflammation, is essential in preventing the progression of related diseases. Your role in addressing inflammation is fundamental to preserving the health and well-being of those you serve.
Acute Vs. Chronic Inflammation

Understanding the nuances between acute and chronic inflammation is crucial, as they represent fundamentally different responses in your body’s defense mechanism. Acute inflammation is an immediate and necessary reaction, involving blood cells called leukocytes that your immune system employs to combat injury or infection. This type of response is characterized by classic signs such as flushed skin, pain, swelling, and heat—symptoms designed to protect and begin the healing process.
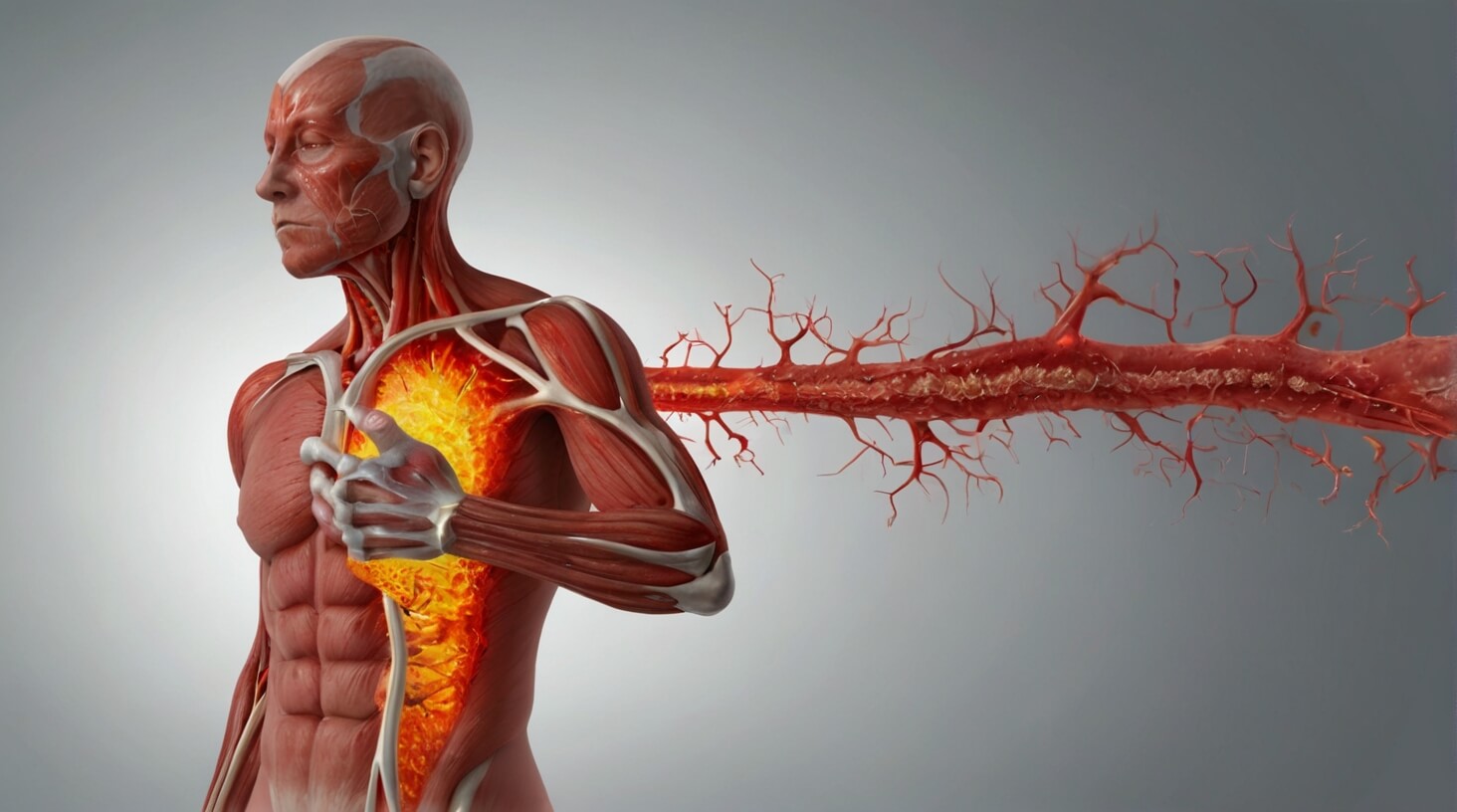
Conversely, chronic inflammation denotes a prolonged and often insidious inflammatory response. Unlike the acute type, which resolves swiftly, chronic inflammation can persist, leading to the gradual deterioration of tissues and organs. This persistent state is associated with a myriad of inflammatory diseases, such as rheumatoid arthritis, which causes severe joint damage, and systemic conditions like heart disease or type 2 diabetes.
Your role in serving others necessitates a comprehensive understanding of these inflammatory processes to effectively reduce inflammation and mitigate the detrimental effects of chronic inflammatory diseases. For instance, recognizing the subtle signs of chronic inflammation—abdominal pain, fatigue, and joint stiffness—can prompt early intervention, which is pivotal in managing conditions like ankylosing spondylitis or Alzheimer’s disease.
Symptoms and Indicators
Recognizing the spectrum of symptoms that signal inflammation, from acute manifestations like swelling and tenderness to chronic indicators such as persistent joint pain, is vital in diagnosing and managing inflammatory conditions effectively. Acute inflammation is your body’s immediate response to injury or infection. It’s orchestrated by the immune system, which deploys immune cells, including white blood cells, to the affected area. This process typically results in:
- Redness and flushed skin due to increased blood flow.
- Pain or tenderness, often signaling that immune cells are active in the area.
- Swelling and heat, a consequence of the fluid and cells accumulating as part of the protective response.
Chronic inflammation, on the other hand, is a prolonged inflammatory response that can play a role in various autoimmune diseases, such as rheumatoid arthritis and inflammatory bowel disease. It is distinguished by a complex set of symptoms and indicators that often include persistent joint pain, skin rashes, and abdominal discomfort. These manifestations might be subtle initially but can become severe over time.
To assess inflammation clinically, healthcare professionals may measure the sedimentation rate of your blood, which indicates the presence of inflammation when elevated. The sedimentation rate is a reflection of how quickly red blood cells settle at the bottom of a test tube; a faster rate suggests an inflammatory process.
Understanding these symptoms and indicators allows you to serve others by identifying potential inflammatory diseases promptly and intervening with appropriate care. By appreciating the nuance between acute and chronic inflammation, you can better support those affected in navigating their path to wellness.
Causes and Triggers
Your body’s immune system can mistakenly target healthy tissues in autoimmune disorders like lupus, sparking an inflammatory response. This is a critical aspect of how inflammation plays a role in certain diseases. In autoimmune conditions, the immune system’s misdirected attacks lead to a cascade of immune responses that cause harm to the body’s own cells.
Exposure to environmental toxins, including pollution and industrial chemicals, can also trigger inflammatory reactions. These chemicals cause the immune system to initiate a defense mechanism, even in the absence of pathogens. The presence of such toxins prompts your body to send signals to the immune system, indicating the need for intervention.
Furthermore, untreated acute inflammation, which may arise from injuries or infections, can transition into chronic inflammation if not resolved. This underscores the importance of the healing process in managing inflammation. When the body sends its defensive cells to the site of damaged tissue, the aim is to eliminate dead tissue and pathogens. However, if this process is disrupted or inefficient, the inflammatory response can become persistent, contributing to the disease process.
Infections, including those that seem minor like the flu, can also set off chronic inflammation. The body’s response to infection is a complicated immune system action designed to isolate and eradicate the invading organisms. Nevertheless, when the inflammation becomes chronic, it can have deleterious effects on the body, leading to further tissue damage.
Lastly, inflammatory processes are central to some types of arthritis, such as rheumatoid arthritis and gouty arthritis. Here, inflammation leads to joint degradation and pain, which are characteristic of these diseases. The persistent inflammation damages the joint structures, causing significant discomfort and reduced mobility. Understanding these triggers is crucial for those who aim to serve others by managing and treating inflammatory conditions.
Treatment and Prevention

To effectively combat inflammation, adopting an anti-inflammatory diet and lifestyle, alongside medical interventions like NSAIDs and corticosteroids, is essential. You must understand that the immune system and immune cells play a critical role in inflammation, which can be both protective and pathological. To lower inflammation, it’s imperative to target these underlying mechanisms through precise, strategic approaches.
Here are three essential strategies to mitigate inflammation:
- Optimize Dietary Choices: You should eat more foods rich in omega-3 fatty acids, such as salmon and flaxseeds, which have potent anti-inflammatory properties. Incorporating a variety of colorful fruits and vegetables into your diet provides antioxidants that support a healthy immune response.
- Implement Lifestyle Modifications: Maintaining a healthy weight, engaging in regular physical activity, and ensuring plenty of sleep are foundational elements that contribute to a healthy lifestyle and can help manage inflammation. Stress reduction techniques, such as meditation and yoga, also have a significant impact on the inflammatory process.
- Utilize Pharmacological Agents: When lifestyle modifications are insufficient, anti-inflammatory drugs (NSAIDs) and corticosteroids may be prescribed to alleviate symptoms. However, these should be used judiciously, as they can have side effects and impact long-term health.
It’s also vital to avoid pro-inflammatory triggers like processed foods, excessive alcohol consumption, and smoking. For individuals with persistent symptoms, seeking medical attention for a tailored treatment plan is crucial. Healthcare providers can offer personalized recommendations to ensure that the approach to managing inflammation is both effective and sustainable. Remember, the goal is not only to treat inflammation but also to prevent its onset through a proactive, informed approach to health.