When you twist your ankle during a morning run, the swelling and redness that follow are signs of acute inflammation, a natural part of your body’s healing process. However, when inflammation becomes chronic, as seen in conditions like rheumatoid arthritis, it’s no longer a fleeting response but a persistent state that can undermine the health of your joints. You’re likely familiar with the discomfort and limited mobility that can accompany inflamed joints, but the underlying mechanisms and long-term consequences may not be as well understood. As you contemplate the complexities of joint inflammation, consider the various factors that contribute to it—ranging from genetic predispositions to environmental triggers—and why a proactive approach to managing inflammation is vital for maintaining not just joint health, but overall well-being. The implications of unchecked inflammation go beyond occasional stiffness or pain; they can shape the trajectory of your physical capabilities and quality of life.
Key Takeaways
- Chronic inflammation can lead to progressive joint damage and pain.
- Inflammatory arthritis is an autoimmune condition that targets the joints.
- Inflammatory cytokines play a role in regulating the intensity and duration of the immune response in arthritis.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and disease-modifying antirheumatic drugs (DMARDs) are common medications used to alleviate symptoms and manage chronic joint pain.
Understanding Joint Inflammation
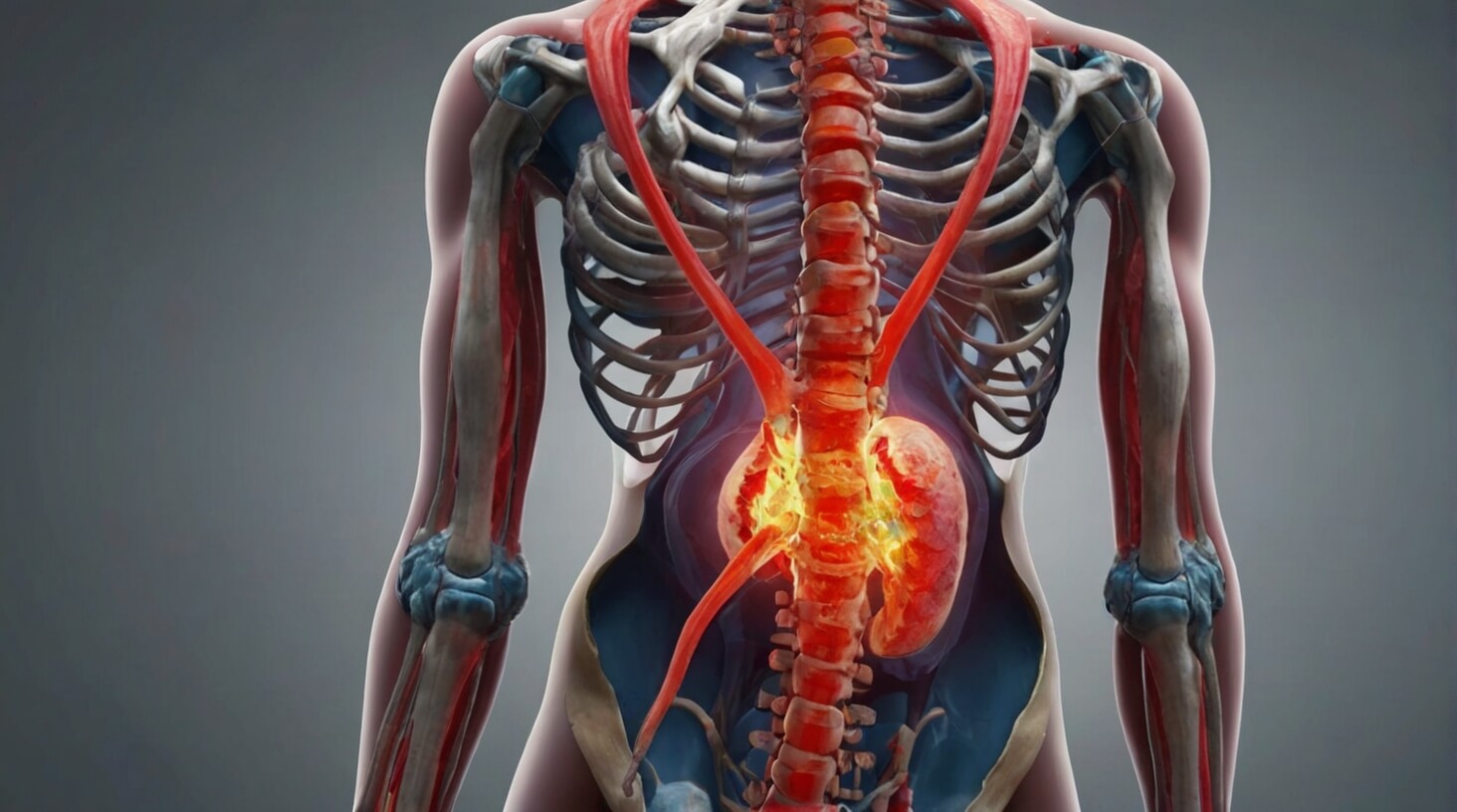
While acute inflammation is a natural response to joint injury or infection, chronic inflammation can lead to progressive joint damage and pain. Your body’s immune system initiates an inflammatory response to combat perceived threats, which can include pathogens, damaged cells, or irritants. This response typically involves the recruitment of inflammatory cells to the affected area to contain and repair the damage.
In the case of inflammatory arthritis, an autoimmune condition, the immune system mistakenly targets the joints, leading to chronic inflammation. This persistent inflammation in the joints can result in the breakdown of cartilage and bone, contributing to the symptoms of joint pain, stiffness, and swelling commonly associated with arthritis.
To mitigate the impact of joint inflammation, it’s important to understand the mechanisms that drive the inflammatory process. Cytokines, small proteins released by inflammatory cells, act as signaling molecules that regulate the intensity and duration of the immune response. In chronic conditions, the sustained presence of inflammatory cytokines fosters a prolonged inflammatory state, further exacerbating joint damage.
Therapeutic strategies to reduce inflammation aim to interrupt this cycle by either suppressing the overall immune response or by targeting specific inflammatory pathways. For instance, nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate the symptoms of joint inflammation by inhibiting enzymes involved in the production of pro-inflammatory mediators. Additionally, disease-modifying antirheumatic drugs (DMARDs) and biologic agents offer more targeted approaches to dampen the immune system’s activity, particularly in arthritis associated with autoimmune dysfunction.
As a caretaker or healthcare provider, your role in managing inflammatory arthritis includes not only administering or advising on pharmacologic interventions but also supporting lifestyle modifications that can help manage chronic inflammation. Regular exercise, a balanced diet, and stress reduction are key factors in maintaining joint health and mitigating the impact of inflammatory conditions.
Causes of Excessive Inflammation

Understanding the mechanisms driving joint inflammation is crucial, and it’s equally important to recognize the underlying causes that can lead to excessive and harmful levels of this response. When your body’s immune response becomes overactive, it can result in chronic inflammatory conditions that manifest as pain, stiffness, and joint damage. Inflammatory arthritis is a prime example of such a condition, with rheumatoid arthritis being one of the most prevalent forms. In rheumatoid arthritis, your immune system mistakenly attacks the synovium—the lining of the membranes that surround your joints—leading to inflammation and joint damage.
Autoimmune diseases are another significant cause of excessive inflammation. These conditions occur when your immune system erroneously targets healthy joint tissue, contributing to the chronic inflammatory process. To manage this, disease-modifying antirheumatic drugs (DMARDs) are often employed, aiming to slow the progression of joint damage and alleviate inflammation caused by the misguided immune response.
In addition to autoimmune triggers, joint inflammation can be instigated by accumulation of crystals, such as uric acid in gout, or calcium pyrophosphate in pseudogout (CPPD). Elevated uric acid levels can cause sharp crystals to form in the joint, triggering intense inflammation and pain.
Moreover, septic arthritis should not be overlooked as a cause of joint inflammation. It is an infection within the joint, typically bacterial, which can quickly and severely inflame the joint space, potentially spreading from a single joint to others if not treated promptly.
Injuries to joints also precipitate inflammation. An acute injury can incite a localized inflammatory response, which sometimes evolves into a chronic condition, especially if the injury is not adequately addressed or if the joint is repeatedly stressed.
Signs and Symptoms
Recognizing the early signs and symptoms of joint inflammation can significantly impact the management and outcome of joint health. When you’re dealing with joint pain, it’s crucial to identify whether inflammation is at play. A common indicator of inflammation is swelling or bulging in the affected joint. This physical manifestation occurs as the immune system responds to what it perceives as threats, leading to an accumulation of fluid.
Pain or aching in the joint, often described as a persistent discomfort, is another red flag. This symptom may intensify during movement or after prolonged inactivity, such as upon waking. Redness or warmth around the joint are also telltale signs of inflammation, resulting from increased blood flow to the area as part of the immune response.
Furthermore, you might experience difficulty moving the affected joint or joints, which can suggest inflammation has compromised joint function. This limitation in mobility often prompts modifications in activities or movement patterns, which can result in pain elsewhere in the body due to compensatory mechanisms.
In the context of chronic conditions like inflammatory arthritis, these symptoms are not fleeting; instead, they represent an ongoing challenge to joint health. Addressing these symptoms effectively often involves a multidisciplinary approach, including physical therapy, to maintain joint function and manage pain.
As someone committed to serving others, it’s imperative to understand that early intervention is key. Encouraging individuals to seek assessment and treatment at the onset of symptoms can prevent further joint damage and enhance quality of life. It’s not just about alleviating pain—it’s about preserving the integrity of the joints for the long term.
Inflammation’s Role in Arthritis
Building on the importance of early intervention in joint inflammation, it’s crucial to explore how persistent inflammation plays a central role in the development and progression of arthritis. Inflammatory arthritis, such as rheumatoid arthritis (RA) and psoriatic arthritis, is not merely a discomfort but a significant threat to joint health. These conditions are evidence of an immune system that’s mistakenly targeting the body’s own tissues.
When the immune system is overactive, it can lead to a cascade of events detrimental to your joints:
- Immune cell infiltration: An overactive immune response can attract immune cells to the joint, causing thickening of the joint lining and swelling in the affected joints.
- Progressive joint damage: Persistent inflammation can damage cartilage, bones, tendons, ligaments, and nerves, leading to irreversible changes.
- Systemic effects: Inflammatory arthritis can also have systemic impacts, affecting organs such as the heart, lungs, and eyes.
- Chronic pain and stiffness: The resulting symptoms include chronic pain and stiffness, which can severely limit mobility and reduce quality of life.
- Treatment with anti-inflammatory medications: To combat these effects and reduce pain, treatment typically includes anti-inflammatory medications aimed at controlling the inflammation and preserving joint function.
It’s essential to understand that inflammation is not just a byproduct but rather a driving force in the pathology of arthritis. The persistent inflammation characteristic of inflammatory arthritis leads to the thickening of the joint lining and subsequent joint damage. This intricate relationship underscores the necessity of prompt and adequate intervention to safeguard joint health and prevent further damage. As someone committed to serving others, recognizing these mechanisms enables you to provide informed care and support to those suffering from arthritis-related inflammation.
Managing Chronic Joint Pain

To effectively manage chronic joint pain, it’s essential to incorporate regular exercise and physical therapy into your routine, as these methods have been proven to alleviate discomfort and enhance joint mobility. A targeted exercise regimen, designed by a healthcare professional, can fortify the muscles surrounding your joints, providing increased support and reducing the strain on the affected areas. Moreover, physical therapy techniques are tailored to your specific condition, promoting flexibility and strength in a controlled and progressive manner.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often recommended by healthcare professionals to manage inflammation and pain associated with conditions like inflammatory arthritis. These medications work by inhibiting enzymes that contribute to inflammation, thereby reducing swelling and discomfort. However, it’s crucial to use NSAIDs judiciously, as they can have side effects, particularly with long-term use.
Beyond medication, lifestyle modifications play a significant role in managing chronic joint pain. Maintaining a healthy weight alleviates extra stress on weight-bearing joints, thus minimizing pain. Stress management techniques also modulate the immune system’s response, potentially decreasing the chronic inflammation characteristic of arthritis.
Utilizing assistive devices can help preserve joint health and function. Ergonomic tools, braces, and supports offer stability, while hot and cold therapies can temporarily soothe pain and reduce swelling. For more persistent cases, healthcare professionals might explore advanced arthritis treatment options, such as corticosteroid injections or disease-modifying antirheumatic drugs (DMARDs), aimed at controlling the immune system and halting the progression of joint damage.
Treatment Options Explored
While managing chronic joint pain often involves a combination of physical therapy and lifestyle adjustments, exploring various treatment options is crucial for effectively reducing inflammation and preserving joint function. As part of your Healthcare Team, you’ll find that a multidisciplinary approach is key, especially in the early stages of inflammatory arthritis or after a joint injury.
When considering pharmacological interventions to reduce inflammation, here’s a list of evidence-based options:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These drugs lower prostaglandin levels, thereby reducing pain and swelling.
- Steroids: Administered orally or through injection, steroids can significantly reduce inflammation and suppress overactive immune responses.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Both nonbiologic and biologic DMARDs are designed to temper the immune system and can be particularly effective for autoimmune types of arthritis.
- Janus Kinase Inhibitors: These newer medications interrupt the transmission of inflammatory signals within the body.
- Lifestyle Modifications: Guided by a physical therapist and other professionals, incorporating regular exercise, dietary changes, stress management, smoking cessation, and adequate sleep can bolster joint health.
You, as someone who strives to serve patients dealing with joint pain, should understand that each treatment option has its place and specificity. Nonbiologic DMARDs, for example, are often the first line of defense in rheumatoid arthritis, while biologics may be reserved for cases that don’t respond to other treatments. Janus kinase inhibitors may be recommended when traditional DMARDs are insufficient. Always work in close collaboration with a physical therapist and the rest of the Healthcare Team to tailor interventions to the individual needs of each patient, ensuring that treatment plans are as effective as possible in managing their joint health.
Lifestyle Adjustments for Relief
Implementing regular exercise into your routine can significantly reduce joint pain and inflammation, representing a cornerstone of non-pharmacological interventions in the management of joint health. Exercise promotes the strengthening of muscles surrounding your joints, enhances bone density, and aids in weight management, which is crucial since excess weight places additional stress on weight-bearing joints, exacerbating inflammatory arthritis symptoms. Furthermore, physical activity increases the production of your body’s natural anti-inflammatory agents, thereby reducing the need for nonsteroidal anti-inflammatory medications.
Beyond exercise, dietary choices play a pivotal role. A healthy diet that avoids processed foods—which often contain pro-inflammatory agents—can help reduce systemic inflammation. Incorporating foods rich in omega-3 fatty acids, antioxidants, and phytochemicals is recommended, as these substances act as natural anti-inflammatory agents.
Stress management is also essential in mitigating inflammation. Chronic stress triggers the release of cortisol, which, when persistently elevated, can impair the body’s ability to regulate inflammation. Techniques such as mindfulness, meditation, and adequate sleep can help regulate your body’s stress response, contributing to improved joint health.
Additionally, lifestyle adjustments such as quitting smoking are recommended, as smoking has been shown to exacerbate inflammation and worsen arthritis symptoms. Professional guidance, such as physical therapy, can provide tailored strategies to maintain mobility and alleviate joint pain.
Future Directions in Joint Health
Building on the foundation of lifestyle adjustments, the scientific community is now exploring advanced interventions and technologies to enhance joint health and combat inflammation more effectively. As you aim to serve patients with inflammatory arthritis, understanding these future directions in joint health is crucial for providing the best care possible.
Innovative therapies are on the horizon, considering the unique genetic and immune system factors that contribute to the types of inflammatory arthritis:
- Personalized Medicine: Advancements in genomics might allow for therapies tailored to an individual’s specific genetic and immune system profile, enhancing the precision with which you can treat inflammatory arthritis.
- Gut Microbiome Research: The gut-joint axis is a promising target for new treatments, potentially preventing or managing inflammation through the modulation of gut microbiota.
- Biomarkers and Imaging: Novel biomarkers and advanced imaging techniques could lead to the earlier identification of ongoing joint inflammation, offering opportunities for timely and personalized interventions.
- Digital Health Technologies: Wearable devices and telemedicine are poised to revolutionize the remote monitoring and management of joint health, increasing patient access to care and improving outcomes.
- Regenerative Medicine: Exploring stem cell therapy and tissue engineering could repair damaged tissues, promoting sustained joint function and health.
These developments represent a significant shift in how medical conditions affecting joints are approached. Your role in understanding and applying these interventions could transform the lives of those battling inflammatory arthritis, ensuring they receive the most cutting-edge, empathetic care available. Keep abreast of these advancements as they promise to redefine the landscape of joint health management.











